Volume 28, Number 12—December 2022
Dispatch
Severe and Rare Case of Human Dirofilaria repens Infection with Pleural and Subcutaneous Manifestations, Slovenia
Cite This Article
Citation for Media
Abstract
We report a case of human Dirofilaria repens infection in a woman in Slovenia who had concomitant pleural and subcutaneous manifestations of the infection. This case report illustrates the clinical course of a severe symptomatic parasitic infection that had multisystemic manifestations.
Dirofilaria repens is a filaria that causes infection primarily in dogs and other wild canids. The infection has been historically endemic in the Mediterranean countries. However, it has expanded to the rest of Europe in the past 2 decades, where it is considered an emerging infection (1).
Canids act as a reservoir for the parasite, where it can reach sexual maturity and produce microfilariae. Microfilariae are ingested by female mosquitoes, where they develop to infective larvae and are introduced to another definitive host during the blood meal of the vector (2). Humans can also acquire the infection, but are considered a dead-end host because microfilaremia in humans has only rarely been demonstrated (3,4).
Clinical symptoms of D. repens infection in humans are the consequence of the inflammatory reaction provoked by the migrating macrofilaria(e). The infection in humans is usually localized with only 1 parasite being found in most cases, and multiple parasites are rarely observed (1,5–7).
Depending on the anatomic location of the symptoms, D. repens infection has traditionally been divided into subcutaneous and ocular forms. The subcutaneous form is characterized by swelling and larva migrans‒like symptoms, whereas the ocular form shows visual disturbances caused by the migrating parasite (1,7,8). In addition, cases of other organ involvement have been reported, including testicles and lungs (1). Another, quite rare form is a pleural form, which manifests as an incidentally detected pleural lesion mimicking malignancy (9).
The course of this infection in humans is usually indolent, except for the ocular form, which can lead to loss of vision and, on rare occasions, involvement of vital organs, such as the central nervous system. Excision of macrofilaria is usually curative because only 1 parasite is usually present. However, in some cases treatment with antiparasitic drugs is needed (10). We report an unusual case in a patient who had pleural and subcutaneous D. repens clinical manifestations.
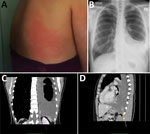
A 40-year-old woman, a nonsmoker who had celiac disease but who was not receiving any regular medication and had no allergies, started having progressive dyspnea, dry cough, pain in the left hemithorax on inspiration, night sweats, and general malaise in September 2020. She reported no fever or weight loss. However, in addition, migratory, angioedematous skin changes measuring ≈15 cm × 15 cm started to appear on the upper trunk and axillary regions. Skin changes were present for 1–3 days and then disappeared (Figure 1, panel A). Her problems gradually intensified during the following months.
The patient sought medical attention in January 2021. Apart from decreased breath sounds on the left side, the clinical examination was unremarkable. Results for complete blood count, leukocyte differential counts, and C-reactive protein level were within reference ranges. A chest radiograph showed left-sided pleural effusion (Figure 1, panel B). Diagnostic thoracocentesis showed exudative pleurisy with lymphocytic predominance. There were no malignant cells, and results of microbiological examinations were negative.
Thorax and abdomen computed tomography scan showed a lesion adjacent to the left posterobasal pleura, pleural thickening suspicious for pleural carcinomatosis, left-sided pleural effusion, and reactive mediastinal and mesenteric lymph nodes (Figure 1, panels C, D).
A video-assisted thoracoscopic surgical excision of the pleural lesion was then performed. A total of 2,000 mL of serohemorrhagic pleural fluid was evacuated during the procedure.
Histologic examination of the excised tissue showed necrotizing granulomas containing structures with a thick, laminated cuticle with external ridges, morphologically characteristic for the Dirofilaria spp. nematode (Figure 2). We extracted DNA from three 10 μm‒thick sections of formalin-fixed, paraffin-embedded tissue block by using a Deparaffinization Solution and a QIAamp DNA Mini Kit (all from QIAGEN, https://www.qiagen.com). D. repens infection was confirmed by using a species-specific, real-time PCR (qPCR), which amplified a 166-bp portion of the cytochrome c oxidase subunit 1 mitochondrial gene (cox1) (11). Sequencing and BLAST analysis (https://blast.ncbi.nlm.nih.gov/Blast.cgi) of a 689-bp fragment of cox1 (12) showed 100% homology with several D. repens isolates from Europe (Figure 3) The sequence obtained has been deposited into GenBank (accession no. OP494268).
To detect microfilaremia, we extracted DNA from an EDTA‒whole blood sample of the patient by using the QIAamp DNA Mini Kit and performed a filarial qPCR, amplifying a portion of the 28S rRNA gene (11). The filarial qPCR result was negative.
Once the diagnosis was established, the patient was asked about possible risk factors for acquisition of the infection. She reported visiting the Istria region in Croatia in March 2020, where she had contact with stray dogs and was bitten by mosquitoes.
After excision of the pleural lesion and evacuation of the pleural fluid, respiratory symptoms of the patient slowly resolved. However, in March 2021, skin lesions persisted, and although not present initially, mild eosinophilia in peripheral blood (0.7 × 109 cells/L) was detected. An ophthalmic examination was performed to exclude the ocular form and showed no abnormality. Treatment with ivermectin (200 μg/kg/d for 4 days) and doxycycline (100 mg 2×/d for 7 days) was initiated.
After treatment, the skin lesions completely disappeared and have not reappeared. The last computed tomography scan of the chest was performed in September 2021 and showed no pleural lesions or pleural effusion and the disappearance or regression of mediastinal and mesenteric lymph nodes. The patient has since remained without any problems.
This case is noteworthy for several reasons. First, it illustrates human D. repens infection with pleural involvement, which is exceedingly rare. In our patient, the infection manifested not only with a pleural lesion but also with large pleural effusion, requiring evacuation of pleural fluid to relieve respiratory symptoms. In general, such clinical manifestations would be suspicious for malignancy, but this possibility was excluded by cytological and histological examinations.
Another filaria, D. immitis, which occurs sporadically in Slovenia and is endemic to neighboring Croatia, can also infect humans and cause predominantly pulmonary symptoms. Without detailed histological examination and molecular diagnosis, this clinical manifestation might be mistaken for D. immitis infection (2).
Second, unlike in most cases, it seems that our patient was infested with >2 macrofilariae, 1 located in the pleura and 1 located in the subcutaneous tissue of the upper body. Clinical manifestation with multiple parasites is rarely encountered in humans and might lead to microfilaremia in some exceptional cases (3–6). Because the filarial qPCR result of a whole blood sample with a detection limit of 1.5 × 10−4 microfilariae/mL of blood (11) was negative, microfilaremia was less probable for our patient.
Presentation with a subcutaneous nodule usually warrants surgical excision, which is diagnostic and curative. However, systemic treatment is needed if macrofilaria(e) cannot be surgically removed. Given the presence of numerous migratory erythematous lesions in our patient, antihelmintic therapy was prescribed.
The prevalence of D. repens infection among dogs in Slovenia is estimated to be 0.64%, whereas in some parts of Croatia it can be as high as 47.3% (13,14). Moreover, there have been case reports of human dirofilariasis in recent years in Slovenia (13,15). It can be assumed that the patient acquired the infection while visiting Croatia, although autochthonous infection cannot be ruled out.
This case illustrates an unusual manifestation of a D. repens nematode infection in a human. Clinicians should become familiar with possible clinical manifestations of this parasitosis, because we can expect an increased number of future cases.
At the time of this study, Dr. Biasizzo was an infectious diseases research scientist at the University Medical Centre, Ljubljana, Slovenia. She is currently an infectious disease resident at the General Hospital, Novo Mesto, Slovenia. Her primary research interests are parasitic diseases, tropical diseases, and infections of the central nervous system.
Acknowledgments
We thank the patient for providing the photograph of the skin lesion and consenting to publication of the case report, Aleš Rode for providing assistance with the laboratory work, and Urška Glinšek Biškup, for assistance with sequencing of the cox1 fragment of D. repens.
This study was partly supported by funding from the Slovenian Research Agency (grant no. P3-0083).
References
- Capelli G, Genchi C, Baneth G, Bourdeau P, Brianti E, Cardoso L, et al. Recent advances on Dirofilaria repens in dogs and humans in Europe. Parasit Vectors. 2018;11:663. DOIPubMedGoogle Scholar
- Simón F, Siles-Lucas M, Morchón R, González-Miguel J, Mellado I, Carretón E, et al. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin Microbiol Rev. 2012;25:507–44. DOIPubMedGoogle Scholar
- Huebl L, Tappe D, Giese M, Mempel S, Tannich E, Kreuels B, et al. Recurrent swelling and microfilaremia caused by Dirofilaria repens infection after travel to India. Emerg Infect Dis. 2021;27:1701–4. DOIPubMedGoogle Scholar
- Lechner AM, Gastager H, Kern JM, Wagner B, Tappe D. Case report: successful treatment of a patient with microfilaremic dirofilariasis using doxycycline. Am J Trop Med Hyg. 2020;102:844–6. DOIPubMedGoogle Scholar
- Sałamatin RV, Pavlikovska TM, Sagach OS, Nikolayenko SM, Kornyushin VV, Kharchenko VO, et al. Human dirofilariasis due to Dirofilaria repens in Ukraine, an emergent zoonosis: epidemiological report of 1465 cases. Acta Parasitol. 2013;58:592–8. DOIPubMedGoogle Scholar
- Simón F, Diosdado A, Siles-Lucas M, Kartashev V, González-Miguel J. Human dirofilariosis in the 21st century: A scoping review of clinical cases reported in the literature. Transbound Emerg Dis. 2022;69:2424–39. DOIPubMedGoogle Scholar
- Ermakova LA, Nagorny SA, Krivorotova EY, Pshenichnaya NY, Matina ON. Dirofilaria repens in the Russian Federation: current epidemiology, diagnosis, and treatment from a federal reference center perspective. Int J Infect Dis. 2014;23:47–52. DOIPubMedGoogle Scholar
- Pupić-Bakrač A, Pupić-Bakrač J, Jurković D, Capar M, Lazarić Stefanović L, Antunović Ćelović I, et al. The trends of human dirofilariasis in Croatia: Yesterday - Today - Tomorrow. One Health. 2020;10:
100153 . DOIPubMedGoogle Scholar - Moskvina TV, Ermolenko AV. Dirofilariasis in Russian Federation: a big problem with large distribution. Russ Open Med J. 2018;7:1–12. DOIGoogle Scholar
- Poppert S, Hodapp M, Krueger A, Hegasy G, Niesen WD, Kern WV, et al. Dirofilaria repens infection and concomitant meningoencephalitis. Emerg Infect Dis. 2009;15:1844–6. DOIPubMedGoogle Scholar
- Laidoudi Y, Davoust B, Varloud M, Niang EHA, Fenollar F, Mediannikov O. Development of a multiplex qPCR-based approach for the diagnosis of Dirofilaria immitis, D. repens and Acanthocheilonema reconditum. Parasit Vectors. 2020;13:319. DOIPubMedGoogle Scholar
- Casiraghi M, Anderson TJC, Bandi C, Bazzocchi C, Genchi C. A phylogenetic analysis of filarial nematodes: comparison with the phylogeny of Wolbachia endosymbionts. Parasitology. 2001;122:93–103. DOIPubMedGoogle Scholar
- Kotnik T, Rataj AV, Šoba B. Dirofilaria repens in dogs and humans in Slovenia. J Vet Res (Pulawy). 2022;66:117–23. DOIPubMedGoogle Scholar
- Tasić-Otašević SA, Trenkić Božinović MS, Gabrielli SV, Genchi C. Canine and human Dirofilaria infections in the Balkan Peninsula. Vet Parasitol. 2015;209:151–6. DOIPubMedGoogle Scholar
- Kramar U, Šoba B, Cvetko B, Cvetko A. First case of ocular dirofilariasis in patient from Slovenia: a case report. In: Klun I, Djurković-Djaković O, editors. Proceedings of the 13th European Multicolloquium of Parasitology; Belgrade, Serbia; October 16‒21, 2021. Belgrade: Bulevar Oslobodjenja; 2021. p. 198.
Figures
Cite This Article1Current affiliation: General Hospital, Novo Mesto, Slovenia.
Table of Contents – Volume 28, Number 12—December 2022
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Helena Biasizzo, General hospital Novo mesto, Šmihelska cesta 1, 8000 Novo mesto, Slovenia
Top