Volume 28, Number 9—September 2022
Research Letter
Pathogenesis and Transmissibility of North American Highly Pathogenic Avian Influenza A(H5N1) Virus in Ferrets
Figure
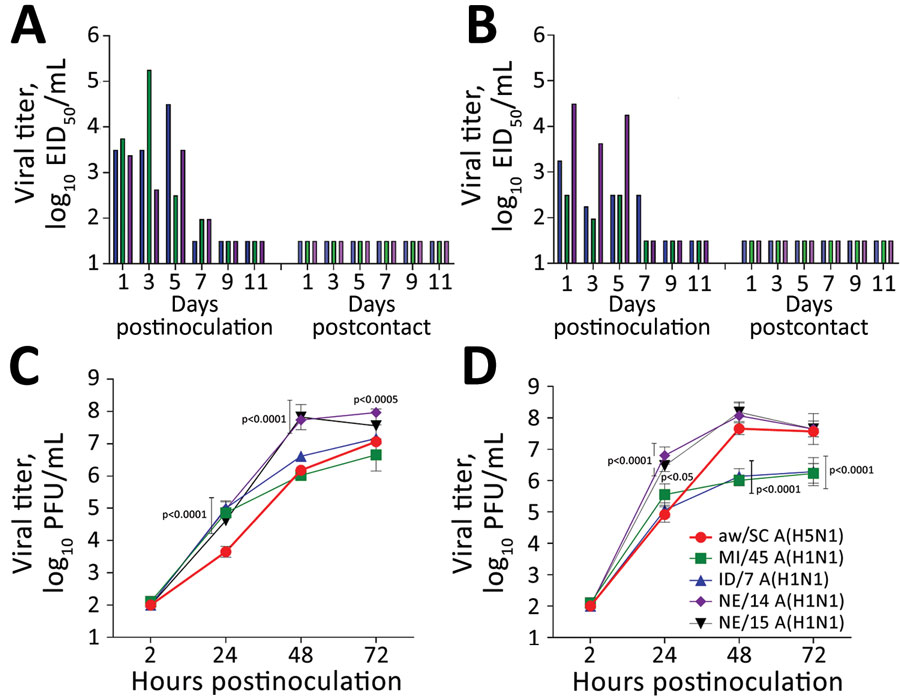
Figure. Evaluating influenza A(H5N1) virus isolate aw/SC using in vivo and in vitro models. A, B) Ferrets were intranasally inoculated with 6 log10 EID50 of aw/SC virus in 1 mL of phosphate-buffered saline and direct contact (A) and respiratory droplet (B) transmission models were established with naive ferrets (1:1 ratio) the following day as described previously (9). Nasal wash samples were collected from inoculated and contact ferrets every other day, and virus titers were determined in eggs (10). As shown, infectious virus was detected in nasal wash specimens from all inoculated ferrets up to day 7 (left side of each panel); however, ferrets exposed only by direct contact (panel A, right) or through the air (panel B, right) did not show infectious virus. C, D) Replication kinetics of aw/SC virus were evaluated in human respiratory tract cells and compared with the H1N1 viruses, A/Michigan/45/2015 (MI/45), A/Idaho/7/2018 (ID/7), A/Nebraska/14/2019 (NE/14), and A/Nebraska/15/2018 (NE/15). Calu-3 cells (ATCC, https://www.atcc.org) were grown to confluence under submerged conditions in 12-mm diameter transwell inserts (Corning, https://www.corning.com). The cells were infected apically at a multiplicity of infection of 0.01 for 1 h and then washed and incubated at 33°C (C) or 37°C (D) as previously described (6). Virus titers in triplicate cell-supernatant samples were determined by standard plaque assay in MDCK cells (10). The limit of virus detection was 1.5 log10 EID50/mL or 2 log10 PFU/mL. Error bars indicate SDs. p values provided for avian H5N1 versus human seasonal H1N1 viruses were calculated by 2-way analysis of variance with a Tukey posttest. aw/SC, A/American Wigeon/SC/22-000345-001/2021; EID50, 50% egg infectious dose.
References
- Lee DH, Torchetti MK, Winker K, Ip HS, Song CS, Swayne DE. Intercontinental spread of Asian-origin H5N8 to North America through Beringia by migratory birds. J Virol. 2015;89:6521–4. DOIPubMedGoogle Scholar
- Wille M, Barr IG. Resurgence of avian influenza virus. Science. 2022;376:459–60. DOIPubMedGoogle Scholar
- Bevins SN, Shriner SA, Cumbee JC Jr, Dilione KE, Douglass KE, Ellis JW, et al. Intercontinental movement of highly pathogenic avian influenza A(H5N1) clade 2.3.4.4 virus to the United States, 2021. Emerg Infect Dis. 2022;28:1006–11. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. US case of human avian influenza A(H5) virus reported. 2022 Apr 28 [cited 2022 Apr 28]. https://www.cdc.gov/media/releases/2022/s0428-avian-flu.html
- Pulit-Penaloza JA, Sun X, Creager HM, Zeng H, Belser JA, Maines TR, et al. Pathogenesis and transmission of novel highly pathogenic avian influenza H5N2 and H5N8 viruses in ferrets and mice. J Virol. 2015;89:10286–93. DOIPubMedGoogle Scholar
- Zeng H, Goldsmith C, Thawatsupha P, Chittaganpitch M, Waicharoen S, Zaki S, et al. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type i interferon response in polarized human bronchial epithelial cells. J Virol. 2007;81:12439–49. DOIPubMedGoogle Scholar
- Nuñez IA, Ross TM. A review of H5Nx avian influenza viruses. Ther Adv Vaccines Immunother. 2019;7:
2515135518821625 . DOIPubMedGoogle Scholar - Centers for Disease Control and Prevention. Summary of Influenza Risk Assessment Tool (IRAT). H5N1 clade 2.3.4.4b [A/American wigeon/South Carolina/AH0195145/2021] [cited 2022 Mar 31]. https://www.cdc.gov/flu/pandemic-resources/monitoring/irat-virus-summaries.htm#H5N122
- Maines TR, Chen LM, Matsuoka Y, Chen H, Rowe T, Ortin J, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci U S A. 2006;103:12121–6. DOIPubMedGoogle Scholar
- Szretter KJ, Balish AL, Katz JM. Influenza: propagation, quantification, and storage. Curr Protoc Microbiol. 2006;15:15G.1.1–1.22.