Volume 28, Number 9—September 2022
Dispatch
Epidemiologic Features and Control Measures during Monkeypox Outbreak, Spain, June 2022
Cite This Article
Citation for Media
Abstract
During June 2022, Spain was one of the countries most affected worldwide by a multicountry monkeypox outbreak with chains of transmission without identified links to disease-endemic countries. We provide epidemiologic features of cases reported in Spain and the coordinated measures taken to respond to this outbreak.
During May‒June 2022, after an alert notification initiated by the United Kingdom (1,2), >4,500 monkeypox cases had been confirmed worldwide, mainly in the European region (3–6). Chains of transmission without links to disease-endemic countries have been identified, and cases have occurred mainly among men who have had sex with men (MSM) in high-risk sexual contexts (5,6).
During June 2022, Spain was one of the countries most affected by monkeypox. We provide epidemiologic features of monkeypox cases reported to the National Surveillance Network through July 4, 2022 (7), complemented with information obtained from bilateral consultations with the Spanish Autonomous Regions, and the measures taken to respond to this alert. No ethics approval was sought because this study describes cases and public health actions in Spain linked to the ongoing multicounty outbreak during June 2022. No personal identifiable data for case-patients or any contacts are included in this report.
Suspected monkeypox cases in Spain were initially reported on May 17. By July 4, of the 19 Autonomous Regions in Spain, 16 had reported 1,256 cases, of which 61.1% (n = 768) were reported by the Region of Madrid. A total of 1,242 cases were in men and 14 in women. The median age of case-patients was 37 years; all but 1 case-patients were adults (Table).
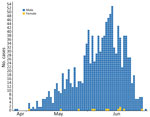
Date of symptom onset was known for 1,182 (89.5%) case-patients . An epidemic plot showed a sustained increasing trend during May and June (Figure). The decreasing numbers during the second half of June might be caused by a delay in reporting.
We obtained information from 4 different series from 4 regions involving 45 patients who self-referred a clear exposure date (range 4‒22 patients/region). This information showed average incubation periods of 7‒9.6 days.
The most frequent symptoms reported (n = 530) were rash (mainly anogenital), fever, asthenia, and lymphadenopathy (Table). Most patients had >1 general symptom plus disseminated and anogenital rash (126 case-patients), >1 general symptom plus anogenital rash (exclusively) (105 case-patients), or >1 general symptom plus diseminated rash (without anogenital or oro/peribuccal location) (76 case-patients). Of the 216 case-patients who had localized lymphadenopathy, 191 had general symptoms. The median number of days from symptom onset to rash was <1 day (IQR 0–2 days; information was available for 427 case-patients). A total of 30 of the 530 case-patients were hospitalized (median admission 2 days); 33 reported complications, mainly secondary bacterial infections (n = 15) oral ulcers (n = 11), proctitis (n = 2), and pharyngotonsillitis (n = 2). No deaths were reported.
Of 440 case-patients who had available information, 62 had traveled to countries that had reported monkeypox cases during the incubation period. A total of 101 case-patients were reported to be close contacts of confirmed or probable case-patients.
The most likely mechanism of transmission reported by 332 (85.8%) of the 387 case-patients who had available information was intimate and prolonged contact during sex. A total of 31 case-patients reported close contacts unrelated to sex; for 24 case-patients, this information was pending. Of those 332 case-patients, 290 were MSM; 6 reported heterosexual contact, and information was pending for the remaining 36. Of 413 case-patients who had available information, 163 had attended a mass gathering before symptom onset; 101 attended Pride events in different cities in Spain. Regarding the 14 women, 7 reported intimate contact during sex with men and 2 had close contacts within the family environment; for 5 women, this information was pending.
A total of 11 regions representing 73% of the case-patients reported provided additional details on contact tracing. It was not feasible to identify or obtain any information regarding potential contacts for a substantial number of patients. Most regions reported an average of <3 identifiable contacts/case-patient. Only 4 regions reported case-patients that had >5 identifiable contacts.
The case definition for monkeypox in Spain considers a confirmed case-patient as a person who had monkeypox genome identified by PCR or who had a positive result in a generic PCR for Orthopoxvirus in a clinical sample. However, the first confirmation of monkeypox cases was conducted by using sequencing (8).
The National Centre for Microbiology conducted partial sequencing of 23 patients and the complete sequencing in samples from 24 cases. This testing identified the West African clade of monkeypox virus.
Following the procedures of the National Early Warning and Rapid Response System, all key stakeholders were alerted to pursue a rapid and coordinated response. A national protocol for early detection and case and contact management was approved and made available by the National Alert Board (8) and coordinated by the Ministry of Health 3 days after detection of suspected cases. A rapid risk assessment for Spain has been reported (9), and situation reports are updated regularly (3). Early consultation and exchange with relevant scientific societies led to publication of an atlas that contained differential diagnoses for monkeypox skin lesions (10).
Partnership with the lesbian, gay, transgender, bisexual, intersex, and queer (LGTBIQ) community was seen as pivotal, and the Ministry of Health involved its Advisory and Counselling Board of nongovernmental organizations in the response to promote the engagement of the LGTBIQ community. In this context, several materials, with key health messages developed, are publicly available (11), building on previous experience on safe sex campaigns, during summer events and following the general principles of the World Health Organization and European Centre for Disease Prevention and Control (12).
Recommendations to offer monkeypox vaccine as postexposure prophylaxis to close contacts, especially those at high risk of developing severe disease and healthcare workers experiencing incidences with the personal protective equipment when in contact with patients, have been proposed by the National Board for Vaccines (13), and >80 contacts (information available from 12 regions) have already been vaccinated. Use of vaccination as preexposure prophylaxis for high-risk groups and healthcare workers with occupational risk is now under discussion as the availability of vaccine increases.
Monkeypox transmission is currently centered, but not exclusively, in MSM who have close physical contact in high-risk sexual contexts. However, without optimal control, there is a risk for transmission to other population groups. Early detection, which requires useful information for the differential diagnosis of clinical manifestations, is crucial to control transmission, as is timely case reporting. It is also essential to continue characterizing the dynamics of the outbreak to identify potential changes to tailor and adapt recommendations.
One of the main challenges encountered in the response to this alert is identifying and tracking contacts: case-patients might be hesitant to provide the identities of their contacts or might not be able to do so because risk exposures had occurred anonymously with previously unknown persons. In certain occasions, it was also difficult to ascertain during the epidemiologic interview the exact date in which transmission might had occurred.
The way the ongoing monkeypox outbreak will evolve is still uncertain and will be influenced by how successfully advice reaches the population at risk. Effective risk communication and community engagement strategies are paramount to delivering information to the general population and to most at-risk persons, including summer mass-gathering event organizers. These features should include clear and contrasted information in partnership with the LGTBIQ community to minimize risk behaviors and maximize awareness about the importance of following public health control measures. Explicit warnings to avoid any form of stigmatizing the LGTBIQ community should frame all interventions.
Dr. Suarez Rodríguez is a Public Health officer at the Coordinating Centre for Health Alerts and Emergencies at the Ministry of Health and head of the Unit on Preparedness and Response, Madrid, Spain. Her primary research interests are epidemiology, surveillance, and public health preparedness and response.
Acknowledgments
We thank all involved scientific societies in Spain for providing consultations, the advisory and counselling boards of nongovernmental organizations for involvement in the alert response, and the Health Centre Sandoval of the Madrid Health Service for collaboration.
Author members of the National Monkeypox Response Group: Coordinating Centre for Health Alerts and Emergencies, Directorate General of Public Health, Ministry of Health: Andrés Mauricio Brandini Romersi, Cristina Giménez Lozano, Alberto Vallejo-Plaza, Gabriela Saravia Campelli, Patricia Santágueda Balader, Lucía García San Miguel, Esteban Aznar Cano; National Centre of Epidemiology, Carlos III Health Institute: Marta Ruiz-Algueró (second affiliation: CIBER in Infectious Diseases, CIBERINFEC), Lorena Simón, Pedro Arias; National Centre for Microbiology, Instituto de Salud Carlos III: Ana Vázquez (second affiliation: CIBER Epidemiologia y Salud Pública, CIBERESP), Patricia Sánchez (second affiliation: CIBER in Infectious Diseases, CIBERINFEC), Laura Herrero, Francisca Molero, Montserrat Torres; Immunization Programme Area, Directorate General of Public Health, Ministry of Health, Madrid, Spain: Laura Sánchez Cambronero Cejudo; División de control de VIH, ITS, Hepatitis Virales y Tuberculosis Ministerio de Sanidad, Madrid, Spain: Rosa Polo, Javier Gómez Castellá, Ana Koerting; Andalucía: Ministry of Health and Families of Andalusia: Isabel Maria Vazquez Rincon; Aragón: Dirección General de Salud Pública: Alberto Vergara Ugarriza, Carmen Montaño Remacha; Asturias: Dirección General de Salud Pública; Gobierno de Asturias: An Lieve Boone, Marta Huerta Huerta; Islas Baleares: Dirección General de Salud Pública. Antonio Nicolau Riutort; Canarias: Dirección General de Salud Pública, Servicio Canario de la Salud: Álvaro Luis Torres Lana, Araceli Alemán Herrera, Isabel Falcón García; Cataluña: Public Health Agency of Catalonia: Manuel Valdivia Guijarro, Gemma Rosell Duran; Ceuta: Consejería de Sanidad, Consumo y Gobernación: Violeta Ramos Marín; Castilla la Mancha: Servicio de Epidemiología de Castilla la Mancha: M. Remedios Rodolfo Saavedra; Castilla y León: Dirección General de Salud Pública: Socorro Fernández Arribas, Henar Marcos Rodríguez, Nuria Rincón Calvo, Virginia Alvarez Rio, Natalia Gutierrez Garzón, Isabel Martínez-Pino (second affiliation: CIBER in Epidemiology and Public Health, CIBERESP, Madrid, Spain), M. Jesús Rodríguez Recio; Comunidad Valenciana: Subdirección General de Epidemiología; Vigilancia de la Salud y Sanidad Ambiental: Francisco Javier Roig Sena; Extremadura: Dirección General de Salud Pública, Servicio Extremeño de Salud: María del Mar López-Tercero Torvisco; Galicia: Sección de Epidemioloxía; Xefatura Territorial de Sanidade, A Coruña: M. del Carmen García Bañobre, Sección de Epidemioloxía. Xefatura Territorial de Sanidade, Pontevedra: M. del Pilar Sánchez Castro, Sección de Epidemioloxía. Xefatura Territorial de Sanidade, Ourense: Miriam Rebeca Martínez Soto; Madrid: Dirección General de Salud Pública. Marcos Alonso García, Fernando Martin Martínez, M Jose Domínguez Rodríguez, Laura Montero Morales, Ana Humanes Navarro, Esther Cordoba Deorador, Antonio Nunziata Forte, Alba Nieto Julia, Noelia Cenamor Largo, Carmen Sanz Ortíz, Natividad García Marín, Jesús Sánchez Díaz, Mercedes Belen Rumayor Zarzuelo, Nelva Mata Pariente, Jose Francisco Barbas del Buey, Manuel Jose Velasco Rodríguez, Andrés Aragón Peña, Elena Rodríguez Baena, Angel Miguel Benito, Ana Perez Meixeira, Jesus Iñigo Martinez, María Ordobas, Araceli Arce; Murcia: Department of Epidemiology, Regional Health Council, IMIB-Arrixaca: Alonso Sánchez-Migallón Naranjo; Navarra: Instituto de Salud Pública de Navarra, Pamplona, Spain, Navarre Institute for Health Research (IdiSNA): Jesús Castilla (third affiliation: CIBER Epidemiologia y Salud Pública, CIBERESP), Itziar Casado (third affiliation: CIBER Epidemiologia y Salud Pública, CIBERESP), Cristina Burgui (third affiliation: CIBER Epidemiologia y Salud Pública, CIBERESP), Nerea Egües, Guillermo Ezpeleta; País Vasco: Departamento de Salud del Gobierno Vasco; Subdirección de Salud Pública y Adicciones de Gipuzkoa: Olatz Mokoroa Carollo (second affiliation: Instituto de investigación Sanitaria Biodonostia); Departamento de Salud del País Vasco, Subdirección de Salud Pública y Adicciones de Araba; Vitoria-Gasteiz: Etxebarriarteun Aranzabal, Larraitz; Departamento de Salud del País Vasco Subdirección de Salud Pública y Adicciones de Bizkaia; Esther Hernandez Arricibita; La Rioja: Dirección General de Salud Pública, Consumo y Cuidados: Ana Carmen Ibáñez Pérez.
References
- UK Health Security Agency. Monkeypox cases confirmed in England: latest updates [cited 2022 Jul 9]. https://www.gov.uk/government/news/monkeypox-cases-confirmed-in-england-latest-updates
- Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, et al. UKHSA Monkeypox Incident Management team. Community transmission of monkeypox in the United Kingdom, April to May 2022. Euro Surveill. 2022;27:
2200422 . DOIGoogle Scholar - Ministry of Health. Situation report. MPX in Spain and other non-endemic countries, June 28, 2022 [in Spanish] [cited 2022 Jul 9]. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/alertaMonkeypox/docs/Informe_de_situacion_MPX_20220610.pdf
- World Health Organization. Multi-country monkeypox outbreak: situation update. June 27, 2022 [cited 2022 Jul 9]. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396
- Joint European Center for Disease Prevention and Control and World Health Organization. Regional Office for Europe Monkepox Surveillance Bulletin, June 29, 2022 [cited 2022 Jun 9]. https://monkeypoxreport.ecdc.europa.eu
- European Centre for Disease Prevention and Control. Monkeypox multi-country outbreak, May 23, 2022. Stockholm; The Centre; 2022 [cited 2022 Jul 9]. https://www.ecdc.europa.eu/sites/default/files/documents/Monkeypox-multi-country-outbreak.pdf
- Carlos III Institute. Information technologies applied to the surveillance of diseases in Spain [in Spanish] [cited 2022 Jul 9]. https://administracionelectronica.gob.es/pae_Home/dam/jcr:35d6af28-9efc-4ae0-81a8-c8ae00cbb52f/48eficiencia.pdf
- Ministry of Health and Carlos III Institute. Protocol for early detection and case management in the context of the MPX alert in Spain, June 10, 2022 [in Spanish] [cited 2022 Jul 9]. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/alertaMonkeypox/docs/20220610_ProtocoloMPX.pdf
- Ministry of Health. Rapid Risk Assessment. Authoctonous cases of monkeypox in Spain and other non-endemic countries [in Spanish] [cited 2022 Jul 9]. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/alertaMonkeypox/docs/ERR_Monkeypox_10062022.pdf
- Spanish Federation of Scientific Medical Associations. Differential diagnosis of monkeypox cutaneous lesions [cited 2022 Jul 9]. https://facme.es/wp-content/uploads/2022/06/01062022-DIAGNOSTICO-DIFERENCIAL-LESIONES-CUTANEAS-.pdf
- Ministry of Health. This year the party is healthy [in Spanish] [cited 2022 Jujl 9]. https://www.sanidad.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/VIRUELADELMONO/esteveranolafiesta.htm
- European Centre for Disease Prevention and Control/World Health Organization Regional Office for Europe. Interim advice for public health authorities on summer events during the monkeypox outbreak in Europe, June 14, 2022 [cited 2022 Jul 9]. https://www.ecdc.europa.eu/sites/default/files/documents/Interim-advice-for-public-health-authorities-on-summer-events-mpx.pdf
- Ministry of Health. Vaccine recommendations in the MPX outbreak [in Spanish] [cited 2022 Jul 9]. https://www.sanidad.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/MonkeyPox/docs/Propuesta_vacunacion_Monkeypox.pdf
Figure
Table
Cite This ArticleOriginal Publication Date: July 12, 2022
1These first authors contributed equally to this article.
2Members of this group are listed at the end of this article.
3These senior authors contributed equally to this article.
Table of Contents – Volume 28, Number 9—September 2022
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Bernardo R. Guzmán Herrador, Coordinating Centre for Health Alerts and Emergencies, Directorate General of Public Health, Ministry of Health, Madrid, Spain
Top