Volume 29, Number 1—January 2023
Dispatch
Successful Treatment of Balamuthia mandrillaris Granulomatous Amebic Encephalitis with Nitroxoline
Figure 1
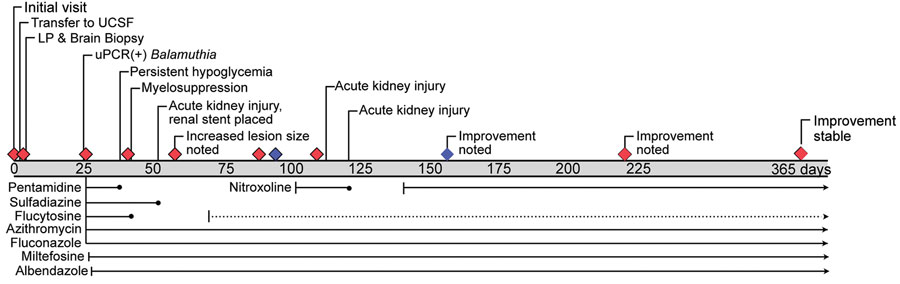
Figure 1. Timeline of events and medications for patient with granulomatous amebic encephalitis, California, USA. Grey bar shows days since initial evaluation; diamonds indicate interval magnetic resonance images; blue diamonds indicate magnetic resonance images taken before and after administration of nitroxoline. Medications at the bottom are other treatments administered. Solid lines refer to the dosages indicated in article text, and dotted lines indicate dose reduction. LP, lumbar puncture; UCSF, University of California, San Francisco Medical Center, San Francisco, California, USA; uPCR, universal broad-range PCR amplicon sequencing.
1These authors contributed equally to this article.
Page created: November 30, 2022
Page updated: December 22, 2022
Page reviewed: December 22, 2022
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.