Volume 29, Number 6—June 2023
Research Letter
Isolated Ocular Mpox without Skin Lesions, United States
Figure
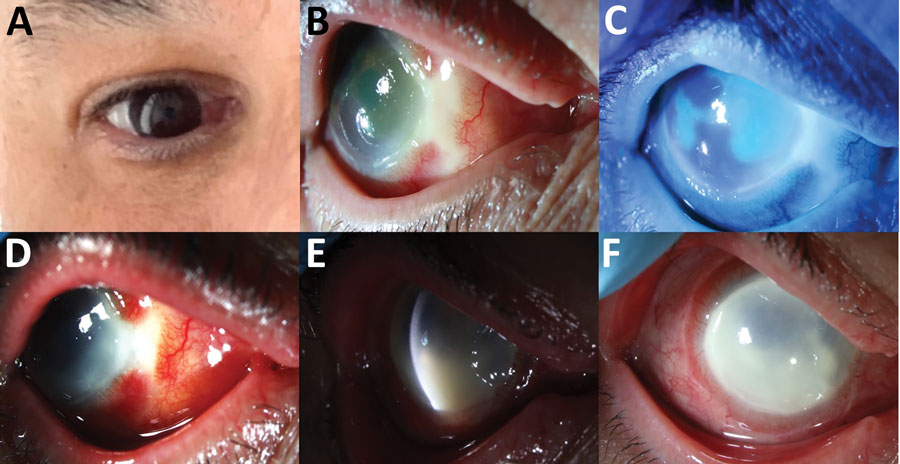
Figure. Clinical progression of ocular mpox in patient in California, USA. A) Initial manifestation of nasal scleral inflammation. B) Nasal scleral necrosis with surrounding scleritis. C) Corneal epithelial sloughing. D) Worsening scleritis and nasal keratitis. E) Corneal endothelial inflammatory plaque. Nasal area of corneal irregularity represents the area of biopsy. F) Progression of diffuse keratitis and corneal limbitis.
Page created: April 26, 2023
Page updated: May 18, 2023
Page reviewed: May 18, 2023
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.