Volume 30, Number 12—December 2024
Dispatch
Human and Canine Blastomycosis Cases Associated with Riverside Neighborhood, Wisconsin, USA, December 2021–March 20221
Cite This Article
Citation for Media
Abstract
We investigated a blastomycosis cluster among humans and canines in a neighborhood in Wisconsin, United States. We conducted interviews and collected serum specimens for Blastomyces antibody testing by enzyme immunoassay. Although no definitive exposure was identified, evidence supports potential exposures from the riverbank, riverside trails or yards, or construction dust.
Blastomycosis, caused by the dimorphic fungus Blastomyces, is a potentially severe disease of humans and animals. Blastomyces favors moist and organically rich soil, and soil disruption can lead to aerosolization and inhalation of infectious Blastomyces conidia (1,2). Most blastomycosis cases in the United States are sporadic and occur in the midwestern, south-central, and southeastern states. Infrequently, clusters of blastomycosis are reported because of common occupational and recreational activities near waterways (3).
In January 2022, St. Croix County Public Health, the Wisconsin Department of Health Services, and the Centers for Disease Control and Prevention (CDC) were notified of a cluster of human and canine blastomycosis cases near the Willow River in St. Croix County, Wisconsin (4). A clinical veterinarian reported 4 canine cases living within a radius of a few miles; 2 cases among persons living in the same area were reported to public health. The multiagency team investigated this cluster to identify risk factors for blastomycosis and to encourage persons in blastomycosis-endemic areas with consistent symptoms to seek healthcare.
The population at risk was defined as persons living within a 1.5-mile diameter of where the human and canine cases occurred. Members of the investigation team administered questionnaires to consenting households (Appendix 1), and collected information on exposures, symptoms, and risk factors for blastomycosis occurring during September 2021–March 2022.
Respondents were eligible to participate in serologic testing; pet owners were offered serologic testing for their dogs. We collected 5–10 mL of venous blood; serum samples were sent to MiraVista Diagnostics (Indianapolis, IN, USA) for Blastomyces spp. IgG testing by enzyme immunoassays (EIA) for human and canine serum samples and by immunodiffusion assay for human serum samples (5). This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.
We defined human cases of blastomycosis among neighborhood residents who had illness onset during September 2021–March 2022. Included residents met clinical case criteria according to the Council of State and Territorial Epidemiologists case definition and met either confirmatory laboratory criteria or presumptive laboratory criteria, including a positive Blastomyces antigen test or a detection of serum antibody through immunodiffusion or EIA (6). Canine cases were dogs that exhibited clinical signs and either had received a diagnosis of blastomycosis from a veterinarian during September 2021–March 2022 or had detectable Blastomyces spp. antibodies.
We described the demographics, recreational exposure history, symptoms, and any symptom-related healthcare visits of persons by clinical case status. We compared recreational exposures between those with antibodies detected (positive or intermediate results) with exposures of those without antibodies detected. Prevalence ratios (PRs) and 95% CIs were calculated using robust Poisson models. All analyses were completed using R version 4.1.3 (The R Project for Statistical Computing, https://www.r-project.org).
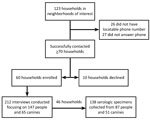
We interviewed members of 60 households, 46 (77%) of whom participated in serologic testing (Figure). The median length of time lived in the neighborhood at time of interview was 4.9 years (range 1 month–56.5 years) (Table 1). The median distance to the in-neighborhood river was 342 (range 1.7–791.0) meters.
During our investigation, 3 previously unreported human cases and 2 additional canine cases of blastomycosis were identified clinically after public health notification to local veterinarians, clinicians, and residents. A total of 5 human and 6 canine cases were included in this investigation (Appendix 2 Tables 1, 2).
The median age among human case-patients was 54 years, and most (60%, n = 3) had >1 comorbidity. All persons reported cough, fever, and fatigue associated with their illness. The initial 2 reported patients were hospitalized, and 1 died (4) (Appendix 2 Table 1). Isolates from the 2 initial cases were sent to the CDC Mycotic Diseases Branch laboratory for species identification, which determined the species to be Blastomyces gilchristii. In the canine cases, 5 of 6 (83%) were in sporting breeds; less than half of participating dogs were sporting breeds (n = 26, 42%). All dogs with a blastomycosis diagnosis were lethargic and anorexic; most had difficulty breathing (83%, n = 5) and cough and fever (67%, n = 4) (Appendix 2 Table 2). Human and canine case exposures varied.
We performed serologic testing on 89 (61%) of 147 human participants and 51 (79%) of 65 dogs (by EIA for dogs and immunodiffusion for humans). A total of 87 persons consented to further testing; their serum samples were later tested by a newly approved EIA. Among persons tested for antibodies, 1 person had detectable Blastomyces antibodies detected by immunodiffusion (also detected by EIA), and 44 (51%) persons had IgG detected by EIA (Table 2). Demographics and recreational exposures did not vary by antibody status, but male participants had 1.5 (95% CI 1.0–2.3) times the prevalence of antibodies than did female participants. Persons who reported a recreational activity involving the in-neighborhood river had 1.5 (95% CI 0.9–2.4) times greater prevalence of detectable antibodies, but was not statistically significant.
Among the 51 dogs tested, 8 (16%) had detectable antibodies, of which 6 (75%) had a clinical diagnosis. Higher number of years lived in the neighborhood was associated with decreased antibody prevalence (PR 0.32; 95% CI 0.1–0.9). Dogs that walked on the trails (PR 10.0; 95% CI 1.3–75.4), specifically those that walked off-leash (PR 6.8; 95% CI 2.0–23.9) had a higher prevalence of antibodies compared with dogs who did not (Table 3). Dogs who lived farther from the river had lower prevalence of antibodies (PR 0.98; 95% CI 0.97–0.99).
We investigated a Wisconsin cluster of blastomycosis in which 5 human cases, resulting in 2 hospitalizations and 1 death, and 6 canine cases were identified. Using a multidisciplinary One Health approach to trigger notification and investigation of this cluster expanded both the investigative team and the outreach and effects among residents, pet owners, veterinarians, construction workers, and healthcare providers. The elevated awareness likely led to additional residents and dogs identified with blastomycosis illness and exposures.
The serological survey revealed nearly half of residents had Blastomyces antibodies detected by EIA. Although this result suggests widespread exposure, the length of time that Blastomyces antibodies remain detectable in the blood and the baseline antibody prevalence in the community are unknown (5,7). Although low sensitivity of immunodiffusion limits its use for detecting antibodies (8), this study used an EIA targeting the BAD-1 antigen with increased sensitivity.
Although we were unable to identify a definitive exposure as the likely cause of this cluster, several sites such as the riverbank, riverside trails or yards, or construction dust, could have plausibly been sources of Blastomyces spores. Although not statistically significant, antibody prevalence was increased in persons who reported participating in activities along the river, as did dogs who walked on in-neighborhood trails (Appendix 2 Tables 3, Figure). Extensive neighborhood construction and excavation during the exposure period might have increased risk for exposure because most recent home construction occurred close to the river. Construction and excavation have been implicated in previous clusters of blastomycosis (9–11).
Prevention of blastomycosis is challenging. Recommendations for persons in blastomycosis-endemic areas include avoiding activities that disrupt dirt and leaf litter and wearing a well-fitted, high-quality facemask during those activities. Immunocompromised persons are at higher risk for severe blastomycosis and should avoid those activities. Risk for blastomycosis cannot be eliminated, and symptoms of blastomycosis can be indistinguishable from other illnesses. Increasing disease awareness is critical to improve early identification and treatment of patients.
Dr. Segaloff is a Career Epidemiology Field Officer with the Centers for Disease Control and Prevention assigned to the Wisconsin Department of Health Services, Madison, Wisconsin. Her research interests include respiratory and emerging infectious diseases surveillance and response.
Acknowledgments
We thank all persons and organizations involved in this investigation, including the New Richmond Veterinary Clinic, Countryside Veterinary Clinic, St. Croix County Public Health, Westfields Hospital Clinical Laboratory, the Wisconsin State Laboratory of Hygiene, the Wisconsin Department of Agriculture, Trade and Consumer Protection, and all neighborhood residents who participated in our investigation. We especially thank the St. Croix County Public Health staff who led the initial case investigation, including Elle Klasen, Lori Peterson, Sue Lindberg, Laurie Diaby, and Jenna Zimmer. We thank those who supplemented our field team, including Lynn Roberts from Wisconsin Department of Health Services, Meredith Smith from Countryside Veterinary Clinic, Bethany Allen from the University of Minnesota, and Martha Pott from Magnusson Veterinary Clinic. We thank Anastasia Livintseva and Joe Sexton for technical assistance and expertise, Andrew Wiese and Andrea Goeldner for their assistance in the initial stages of the investigation, and the GIS Team for their assistance with the spatial analyses.
A.H. and K.C. are both employed by MiraVista Diagnostics. The test used in this investigation is offered commercially by MiraVista Diagnostics.
References
- Sarosi GA, Hammerman KJ, Tosh FE, Kronenberg RS. Clinical features of acute pulmonary blastomycosis. N Engl J Med. 1974;290:540–3. DOIPubMedGoogle Scholar
- Klein BS, Vergeront JM, Weeks RJ, Kumar UN, Mathai G, Varkey B, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986;314:529–34. DOIPubMedGoogle Scholar
- Benedict K, Gibbons-Burgener S, Kocharian A, Ireland M, Rothfeldt L, Christophe N, et al. Blastomycosis surveillance in 5 states, United States, 1987–2018. Emerg Infect Dis. 2021;27:999–1006. DOIPubMedGoogle Scholar
- Segaloff HE, Wu K, Shaw S, Klasen EM, Peterson L, Lindberg S, et al. Notes from the field: cluster of blastomycosis among neighborhood residents—St. Croix County, Wisconsin, 2022. MMWR Morb Mortal Wkly Rep. 2023;72:348–9. DOIPubMedGoogle Scholar
- Mourning AC, Patterson EE, Kirsch EJ, Renschler JS, Wolf LA, Paris JK, et al. Evaluation of an enzyme immunoassay for antibodies to a recombinant Blastomyces adhesin-1 repeat antigen as an aid in the diagnosis of blastomycosis in dogs. J Am Vet Med Assoc. 2015;247:1133–8. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Blastomycosis 2020 case definition [cited 2024 Feb 5]. https://ndc.services.cdc.gov/case-definitions/blastomycosis-2020
- Spector D, Legendre AM, Wheat J, Bemis D, Rohrbach B, Taboada J, et al. Antigen and antibody testing for the diagnosis of blastomycosis in dogs. J Vet Intern Med. 2008;22:839–43. DOIPubMedGoogle Scholar
- Klein BS, Vergeront JM, DiSalvo AF, Kaufman L, Davis JP. Two outbreaks of blastomycosis along rivers in Wisconsin. Isolation of Blastomyces dermatitidis from riverbank soil and evidence of its transmission along waterways. Am Rev Respir Dis. 1987;136:1333–8. DOIPubMedGoogle Scholar
- Frye MD, Seifer FD. An outbreak of blastomycosis in eastern Tennessee. Mycopathologia. 1991;116:15–21. DOIPubMedGoogle Scholar
- Kitchen MS, Reiber CD, Eastin GB. An urban epidemic of North American blastomycosis. Am Rev Respir Dis. 1977;115:1063–6.PubMedGoogle Scholar
- Tosh FE, Hammerman KJ, Weeks RJ, Sarosi GA. A common source epidemic of North American blastomycosis. Am Rev Respir Dis. 1974;109:525–9.PubMedGoogle Scholar
Figure
Tables
Cite This ArticleOriginal Publication Date: November 20, 2024
1The results of this investigation were presented at the Council for State and Territorial Annual Conference, June 25–29, 2023; Salt Lake City, Utah, USA.
2These senior authors contributed equally to this article.
Table of Contents – Volume 30, Number 12—December 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Suzanne Gibbons-Burgener, 1 West Wilson St, Rm 272, Madison, WI 53703, USA
Top