Volume 31, Number 8—August 2025
Dispatch
Neurologic Manifestations Associated with Parvovirus B19 Epidemic, Madrid, Spain, 2024
Abstract
A reemergence of parvovirus B19 infections in Spain in early 2024 prompted a 10-year review of the virus at a tertiary center. We identified 8 case-patients with neurologic manifestations who had parvovirus B19 in cerebrospinal fluid. Early recognition and management of parvovirus B19–associated neurologic conditions will help yield favorable outcomes.
Parvovirus B19 is a small, nonenveloped DNA virus that belongs to the Parvoviridae family. Parvovirus B19 infection generally manifests in paucisymptomatic or mild forms (1,2). However, severe symptoms, including chronic anemia, pancytopenia, and transient aplastic crisis, have been observed in at-risk populations, such as pregnant women, immunocompromised patients, and persons with chronic hematologic diseases. Neurologic manifestations of parvovirus B19 are rarely documented, underscoring the necessity for further epidemiologic and clinical investigation (2,3).
Community parvovirus B19 outbreaks typically peak in winter and spring and last an average of 3–6 months (4). Because parvovirus B19 is a nonnotifiable disease, testing practices vary between countries. Pregnant women and immunocompromised patients represent special cases for which testing is common (1).
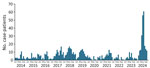
Since March 2024, many countries in Europe, including Spain, have reported increased detection of parvovirus B19 (1). We observed a similar trend at Hospital Gregorio Marañón in Madrid, Spain, and we saw a larger peak of cases in the 2024 outbreak compared with the previous 10 years (Figure 1). After the reemergence of parvovirus B19, we observed the virus in cerebrospinal fluid (CSF) in some patients from our center. We investigated the clinical features and microbiological findings from case-patients with neurologic symptoms treated at Hospital Gregorio Marañón during 2014–2024.
We conducted a retrospective data extraction on CSF samples submitted to our laboratory for diagnostic workup of meningoencephalitis during January 2014–October 2024. We excluded bacterial and other viral causes of meningoencephalitis by using bacterial culture and molecular tests. We performed a review of demographic and clinical features on patients with CSF samples positive for parvovirus B19. We included serologic data when available by using an Alinity i System chemiluminescence assay (Abbott Laboratories, https://www.abbott.com). We performed molecular testing on CSF by using Allplex Meningitis V1-V2 Panel Assays multiplex PCR (Seegene, http://www.seegene.com) (Appendix). To ensure accuracy, we performed a second parvovirus B19–specific PCR on case-patients with virus detected in the central nervous system during 2024. For plasma samples, we used a specific target PCR (RealStar Parvovirus B19 PCR Kit; Altona Diagnostics, https://www.altona-diagnostics.com) and performed diagnostic testing procedures using the manufacturer’s specifications. Since 2019, our laboratory has been equipped with multiplex PCR for CSF; before 2019, we outsourced that test to the national reference laboratory in Madrid.
During the January–October 2024 outbreak, we found 6 of 223 CSF samples tested were positive for parvovirus B19. An archival review of meningoencephalitis cases tested during 2014–2023 revealed 2 of 801 additional hospital patients with parvovirus B19 in CSF. The overall CSF parvovirus B19 positivity rate for the entire 10-year period was 0.8% (8 patients): 6 patients had no underlying immunosuppression, but the other 2 had a history of hematologic disease (Table; Figure 2). No cutaneous manifestations were observed. Central nervous system manifestations exhibited variability, and mental status changes were the most common. CSF analysis showed protein levels greater than the upper reference limit (i.e., >30 mg/dL) in all samples. Three patients received a 5-day course of intravenous immunoglobulin (IVIg), but no clinical benefit was observed between treated and untreated patients. All patients recovered completely without neurologic sequelae (range 3–21 days). Brain magnetic resonance imaging and computed tomography scans were unremarkable; the exception was case-patient 5, in whom a parenchymal lesion observed on the brain computed tomography scan was consistent with a high-grade lymphoproliferative disease. We performed cytology and confirmed lymphoproliferative disease (Appendix).
This study lends support to the numerous reports indicating a rise of parvovirus B19 infection during the 2024 outbreak compared with previous years (1,5,6). However, the precise causes of the increase in case numbers remain unclear. Although a multitude of factors are likely implicated, reduced host immune response attributable to restrictions during the COVID-19 pandemic period warrants consideration. Moreover, the absolute increase in case numbers could result in a proportional rise of symptomatic cases, and some cases might have more severe clinical manifestations.
The association between parvovirus B19 infection and neurologic symptoms is poorly documented. Cases of parvovirus B19 infection in persons exhibiting neurologic manifestations are not distinguishable from cases of encephalitis caused by other viral agents. The proposed physio-pathologic mechanisms contributing to the development of neurologic manifestations during parvovirus B19 infection are complex and variable. Those mechanisms include direct viral toxicity, dysregulated immune responses with the release of cytokines in the CSF, immune complex deposition on endothelial cells, and intracellular accumulation of the toxic nonstructural 1 protein (5,7).
Some studies reported findings that support parvovirus B19 infection as a cause of neurologic manifestations. A comprehensive review identified 129 cases related to parvovirus B19 infection and neurologic symptoms; one third of the patients had a previous history of altered immunity (2). Another study found the most common parvovirus B19–associated neurologic manifestation was encephalitic syndromes (39%) (8). Rash was observed more frequently among immunocompetent patients than in those with altered immunity; in some cases, rash preceded the onset of other clinical findings (2,8). Arthralgia or arthritis symptoms were infrequent. CSF alterations did not show a clear pattern; the median leukocyte count was 9 cells/mL, and a slight increase in protein levels (51%) was the most notable finding. Up to 42% of cases had hematologic disturbances (2,8).
In our case series, parvovirus B19 infection manifested in the absence of typical cutaneous manifestations. Among patients in our study, thrombocytopenia was the most prevalent hematologic disorder, and analysis of CSF samples revealed protein levels greater than the established threshold in all cases. In addition, most cases in our study were among adults without underlying immunocompromising diseases.
Parvovirus B19 is frequently underestimated in differential diagnosis schemes of meningoencephalitis. To accurately diagnose parvovirus B19 infection when neurologic involvement is observed, use of additional microbiological investigations is recommended, including serologic markers and virus DNA analysis in plasma and CSF.
In terms of management, steroids and IVIg have been identified as treatment options for clinical syndromes linked to parvovirus B19 infection. The choice to use IVIg is based on the assumption that it contains a substantial quantity of antibodies capable of neutralizing the virus. However, the precise mechanism of IVIg action remains uncertain (2,8). We did not observe any clinical differences between the patients who received IVIg and those who did not. The prognosis for neurologic manifestations associated with parvovirus B19 seems favorable; we saw a high rate of spontaneous recovery and an absence of sequelae. Nevertheless, long-term neurologic effects have been documented, including bradyphemia (slow speech), learning difficulties, and slurred speech, as well as more severe outcomes, such as mental and motor impairment and death (2,8). In this particular context, our findings are consistent with the available literature on parvovirus B19 infections with neurologic manifestations.
This study is limited by its retrospective design, single institution data collection, and small sample size of neurologic parvovirus B19 infections, which might bias the ability to draw definitive conclusions. Nevertheless, this study furnishes valuable information regarding viral determination in the CSF, thereby enabling the formulation of subsequent hypotheses and research initiatives.
Our findings underscore the importance of incorporating parvovirus B19 into differential diagnoses of encephalitis, given its capacity to affect both immunocompetent and immunocompromised persons. Research is needed to elucidate the underlying mechanisms of parvovirus B19 to develop targeted treatments. Early recognition and appropriate management of parvovirus B19–associated neurologic conditions have the potential to yield favorable outcomes.
Dr. Veintimilla is a clinical microbiologist in the Department of Clinical Microbiology and Infectious Diseases at the Gregorio Marañón Hospital in Madrid, Spain. Her research interests include molecular diagnostics and infections in immunosuppressed hosts.
Acknowledgments
We thank Lara Mesones Guerra and Sandra Rodrigo for contributing to the processing of samples for the B19V diagnostics.
C.V. and M.V. conceptualized the study. C.V., P.C., A.E., and R.A. provided data and performed data analyses. C.V. drafted the original manuscript. P.C., R.A., M.V., and P.M. supervised the data interpretation and revised the first draft. P.C., A.E., R.A., M.V., and P.M. contributed to critical reviewing and editing the manuscript. All authors have read and approved the final manuscript for publication.
References
- European Centre for Disease Prevention and Control. Risks posed by reported increased circulation of human parvovirus B19 in the EU/EEA–5 June 2024. Stockholm: The Centre; 2024.
- Douvoyiannis M, Litman N, Goldman DL. Neurologic manifestations associated with parvovirus B19 infection. Clin Infect Dis. 2009;48:1713–23. DOIPubMedGoogle Scholar
- Eid AJ, Ardura MI, Infectious Diseases AST; AST Infectious Diseases Community of Practice. Human parvovirus B19 in solid organ transplantation: Guidelines from the American society of transplantation infectious diseases community of practice. Clin Transplant. 2019;33:
e13535 . DOIPubMedGoogle Scholar - Cherry J, Demmler-Harrison GJ, Kaplan SL, Steinbach WJ, Hotez P. Feigin and Cherry’s textbook of pediatric infectious diseases, 8th edition. New York: Elsevier; 2017.
- Russcher A, van Boven M, Benincà E, Verweij EJTJ, Molenaar-de Backer MWA, Zaaijer HL, et al. Changing epidemiology of parvovirus B19 in the Netherlands since 1990, including its re-emergence after the COVID-19 pandemic. Sci Rep. 2024;14:9630. DOIPubMedGoogle Scholar
- Barah F, Vallely PJ, Cleator GM, Kerr JR. Neurological manifestations of human parvovirus B19 infection. Rev Med Virol. 2003;13:185–99. DOIPubMedGoogle Scholar
- Nordholm AC, Trier Møller F, Fischer Ravn S, Flink Sørensen L, Moltke-Prehn A, Elskær Mollerup J, et al. Epidemic of parvovirus B19 and disease severity in pregnant people, Denmark, January to March 2024. Euro Surveill. 2024;29:
2400299 . DOIPubMedGoogle Scholar - Barah F, Whiteside S, Batista S, Morris J. Neurological aspects of human parvovirus B19 infection: a systematic review. Rev Med Virol. 2014;24:154–68. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleOriginal Publication Date: July 14, 2025
Table of Contents – Volume 31, Number 8—August 2025
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Cristina Veintimilla, Hospital General Universitario Gregorio Marañón, 46 C/Doctor Esquerdo, 28007 Madrid, Spain
Top