Volume 31, Number 8—August 2025
Dispatch
Progression from Candida auris Colonization Screening to Clinical Case Status, United States, 2016–2023
Cite This Article
Citation for Media
Abstract
During 2016–2023, among 21,195 US patients who tested positive for Candida auris colonization, 6.9% were subsequently found to have a positive clinical specimen (2.8% from blood). Strategies are needed to prevent invasive C. auris infections among patients with colonization (e.g., through patient decolonization).
Candida auris, an emerging, frequently antifungal-resistant yeast, can colonize patients asymptomatically and persist on skin for months to years without causing infection (1–3). Patients colonized with C. auris can progress to having invasive infections, which are associated with crude mortality rates of 30%–72% (4,5). Because C. auris spreads easily in healthcare settings, the Centers for Disease Control and Prevention (CDC) recommends colonization screening for patients with high-risk healthcare exposures (e.g., recent stay in a long-term acute-care hospital [LTACH] or ventilator-capable skilled nursing facility [SNF]) and those with an epidemiologic link to a patient with C. auris (2,6) (https://www.cdc.gov/candida-auris/hcp/screening-hcp).
Data characterizing the progression from C. auris colonization to invasive disease are limited but might help guide public health surveillance, prevention, and treatment efforts. We analyzed US national case-based surveillance data to characterize patients with positive C. auris screening results who were subsequently found to have a positive clinical specimen.
C. auris is a nationally notifiable condition, but reporting mandates vary across states and jurisdictions. State and jurisdictional health departments report C. auris screening and clinical cases to CDC. Screening cases were defined as a positive C. auris laboratory result from a swab sample (usually composite axilla/groin) collected to test for colonization. Clinical cases were defined as a positive C. auris laboratory result from a clinical specimen collected to determine the cause and treatment for infection in a patient. Clinical cases might involve body sites typically associated with invasive infection (e.g., blood) or those that potentially reflect colonization (e.g., urine) (https://ndc.services.cdc.gov/case-definitions/candida-auris-2023). Screening and clinical case data included information on patient age and sex, as well as date and facility type of specimen collection. Facility location was grouped by Antimicrobial Resistance Laboratory Network region (n = 7) (https://www.cdc.gov/antimicrobial-resistance-laboratory-networks/php/about/domestic.html). We used a patient-level identifier to link each patient’s screening case with a clinical case, if one occurred. We considered patients with the corresponding clinical case >1 calendar day after a screening case to have a screening-to-clinical (StC) event.
The analysis includes each patient’s screening case on the basis of their first positive screening result (StC and non-StC events) and clinical case on the basis of first positive clinical specimen (StC events only) during 2016–2023. We calculated total and annual percentages of patients with screening cases who had StC events and described available data on non-StC events and StC events, stratifying by StC event status and examining StC events by body site involved. We analyzed categorical data using χ2 tests and continuous data using Kruskal-Wallis rank-sum tests (α = 0.05).
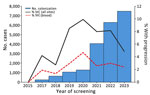
During 2016–2023, a total of 36 of 40 reporting jurisdictions reported 21,195 patients who had a positive screening result; of those, 1,458 (6.9%) patients across 22 jurisdictions had an StC event (2.8% blood, 4.1% nonblood) (Table 1). The number of patients with screening cases increased each year, and the percentage of those with an StC event increased from 0.0% (0/13) in 2016 to 9.9% (129/1,299) in 2020, then decreased to 4.9% (365/7,493) in 2023 (Figure 1).
Among patients with screening cases (n = 21,195), the median age was 68 (interquartile range [IQR] 58–76) years; of those with known sex (n = 16,446), 9,448 (57.4%) were men and 6,998 (42.6%) were women (Table 1). The most common regions of screening case specimen collection were the West (31.2%, n = 6,617), Midwest (20.1%, n = 4,264), and Southeast (20.0%, n = 4,235) and the most common facility types among those with known facility type (n = 17,357) were LTACH (50.2%, n = 8,716), acute care hospital (ACH) (29.0%, n = 5,033), and ventilator-capable SNF (16.8%, n = 2,912). StC event frequency was similar by age (p = 0.650) and sex (p = 0.478) and varied by region (p<0.001), and facility type (p<0.001). StC event frequency was similar between women (7.4%) and men (7.1%) and was greatest among patients with screening specimens collected in the West (13.6%), Northeast (8.5%), Mid-Atlantic (4.3%), or Mountain (4.3%) regions. StC events were most frequent for patients with screening specimens collected in LTACHs (10.4%), then ACHs (5.9%), ventilator-capable SNFs (5.2%), non–ventilator-equipped SNFs (2.7%), and other facility types (1.9%).
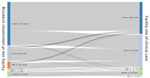
Among StC events (n = 1,458), blood (40.1%, n = 584) and urine (26.8%, n = 391) were most common (Table 2); the distribution of affected body sites was generally similar across years (Appendix Figure). Body sites of clinical cases varied by age (p = 0.023), sex (p<0.001), region (p<0.001), and time from screening case to clinical case specimen collection (p = 0.001) (Table 2). Among women, blood specimens were approximately twice as common as urine (42.6% vs. 21.5%), whereas among men, the percentage was similar (32.0% vs. 32.2%). Blood specimens constituted most StC events in the Southeast (58.9%), Northeast (58.6%), and Mid-Atlantic (57.8%) regions but less than half of specimens in other regions. The median number of days from initial screening case specimen to clinical specimen was longest for blood (58, IQR 22–130, range 1–1,309 days) and shortest for respiratory (33, IQR 17–74, range 1–1,240 days) and other (28, IQR 14–77, range 1–745 days) specimen types. The most common facility types of initial screening case detection were LTACHs (62.2%) and ACHs (20.5%) (Figure 2). Regardless of the facility type where the screening case was detected, most StC events were detected in an LTACH (45.6%) or ACH (46.0%).
This analysis of national C. auris case data revealed that, among 21,195 patients who tested positive for C. auris on a colonization screening swab during 2016–2023, a clinical case subsequently occurred in 6.9% (2.8% involving blood); more than half of clinical cases involving blood were detected 2 months after screening case detection. This finding is comparable with a smaller New York state study in which a C. auris bloodstream infection occurred in 7/187 (3.7%) colonized patients (median time from screening case testing to infection 86 days) (7).
The percentage of patients with an StC event peaked in 2020 then declined, potentially because of improved infection prevention and control efforts or increased screening after COVID-19–related resource strains resolved. The volume of screening cases and frequency of clinical cases was greatest in the West, but the region had a relatively low percentage of clinical cases involving blood; that finding might reflect regional differences in case reporting and in testing practices for C. auris in noninvasive body sites (8). Most StC events were identified in LTACHs and ACHs, underscoring the continued need for focused screening, enhanced surveillance, and efforts to improve infection prevention and control implementation in these settings.
For several reasons, we suspect that our study underestimates the actual percentage of patients with C. auris colonization who progress to having a clinical case. StC events could have been missed because of missed screening opportunities, the insensitivity of culture (9), treating clinical laboratories that might not routinely distinguish C. auris from other Candida species for nonsterile specimen types (10), and the fact that US C. auris data from 2024 are not finalized, meaning some patients might not have had sufficient lead time for clinical cases to occur. In addition, for clinical cases, we lacked data on previous negative screening results, the differentiation between infection and colonization, and underlying patient conditions.
Overall, our study highlights the potential for C. auris infections, particularly candidemia, among patients colonized with C. auris. Rigorous infection prevention and control remain necessary to prevent the spread of C. auris and subsequent clinical infections. Further studies could investigate risk factors and strategies to prevent invasive C. auris infections among patients with colonization (e.g., through patient decolonization).
Ms. Baker is an epidemiologist with the Mycotic Diseases Branch, Division of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA. Her research interests include the epidemiology and prevention of fungal infections.
Acknowledgments
We thank Malavika Rajeev for providing guidance on data management and informatics and the CDC Antimicrobial Resistance Laboratory Network in providing testing for C. auris detection and drug susceptibility.
This activity was reviewed by the CDC Institutional Review Board, deemed not research, and was conducted consistent with applicable federal law and CDC policy (see e.g., 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
References
- Lyman M, Forsberg K, Sexton DJ, Chow NA, Lockhart SR, Jackson BR, et al. Worsening spread of Candida auris in the United States, 2019 to 2021. Ann Intern Med. 2023;176:489–95. DOIGoogle Scholar
- Pacilli M, Kerins JL, Clegg WJ, Walblay KA, Adil H, Kemble SK, et al. Regional emergence of Candida auris in Chicago and lessons learned from intensive follow-up at 1 ventilator-capable skilled nursing facility. Clin Infect Dis. 2020;71:e718–25. DOIGoogle Scholar
- Arenas SP, Persad PJ, Patel S, Parekh DJ, Ferreira TBD, Farinas M, et al. Persistent colonization of Candida auris among inpatients rescreened as part of a weekly surveillance program. Infect Control Hosp Epidemiol. 2024;45:762–5. DOIGoogle Scholar
- Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017;64:134–40. DOIGoogle Scholar
- Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M, et al. Incidence, characteristics and outcome of ICU-acquired candidemia in India. Intensive Care Med. 2015;41:285–95. DOIGoogle Scholar
- McKinnell JA, Singh RD, Miller LG, Kleinman K, Gussin G, He J, et al. The SHIELD Orange County Project: multidrug-resistant organism prevalence in 21 nursing homes and long-term acute care facilities in southern California. Clin Infect Dis. 2019;69:1566–73. DOIGoogle Scholar
- Southwick K, Adams EH, Greenko J, Ostrowsky B, Fernandez R, Patel R, et al. New York state 2016–2018: progression from Candida auris colonization to bloodstream infection. Open Forum Infect Dis. 2018;5(suppl_1):S594–5. DOIGoogle Scholar
- Lockhart SR, Jackson BR, Vallabhaneni S, Ostrosky-Zeichner L, Pappas PG, Chiller T. Thinking beyond the common Candida species: need for species-level identification of Candida due to the emergence of multidrug-resistant Candida auris. J Clin Microbiol. 2017;55:3324–7. DOIGoogle Scholar
- Clancy CJ, Nguyen MH. Finding the “missing 50%” of invasive candidiasis: how nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin Infect Dis. 2013;56:1284–92. DOIGoogle Scholar
- Keighley C, Garnham K, Harch SAJ, Robertson M, Chaw K, Teng JC, et al. Candida auris: diagnostic challenges and emerging opportunities for the clinical microbiology laboratory. Curr Fungal Infect Rep. 2021;15:116–26. DOIGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: July 10, 2025
Table of Contents – Volume 31, Number 8—August 2025
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Anna Baker, Centers for Disease Control and Prevention, 1600 Clifton Rd NE, Mailstop 17-02, Atlanta, GA 30329-4018, USA
Top