Volume 5, Number 3—June 1999
Synopsis
Q Fever in Bulgaria and Slovakia
Cite This Article
Citation for Media
Abstract
As a result of dramatic political and economic changes in the beginning of the 1990s, Q-fever epidemiology in Bulgaria has changed. The number of goats almost tripled; contact between goat owners (and their families) and goats, as well as goats and other animals, increased; consumption of raw goat milk and its products increased; and goats replaced cattle and sheep as the main source of human Coxiella burnetii infections. Hundreds of overt, serologically confirmed human cases of acute Q fever have occurred. Chronic forms of Q fever manifesting as endocarditis were also observed. In contrast, in Slovakia, Q fever does not pose a serious public health problem, and the chronic form of infection has not been found either in follow-ups of a Q-fever epidemic connected with goats imported from Bulgaria and other previous Q-fever outbreaks or in a serologic survey. Serologic diagnosis as well as control and prevention of Q fever are discussed.
Q fever, a widespread zoonosis recognized as a clinical entity in 1937 (1), is caused by the obligate intracellular parasite, Coxiella burnetii. The disease is endemic worldwide, occurring in different geographic regions and climatic zones (2). New Zealand is probably the only large country without Q fever (3). The principal vectors of C. burnetii are ticks, which transmit the agent to wild animals (causing wildlife coxiellosis) or to domestic animals (creating the livestock reservoir of C. burnetii) (4). The most important reservoirs in nature are small wild rodents, but infection was also demonstrated in insectivores, lagomorphs, carnivores, ungulates, ruminants, marsupials, monkeys, bats, birds, and even reptiles and fish (5,6). Infected domestic animals (cattle, sheep, and goats but also pet animals, especially cats), frequently with persistent and subclinical coxiellosis, represent the main source of C. burnetii infection for humans, who become infected by direct contact with these animals, by environmental contamination (from animal excrements), and (indirectly) through processing or consuming animal products. Human infection is acquired most often by the inhalation of contaminated aerosols but may also occur through the digestive tract, through skin trauma, or by sexual contact. Mother-to-fetus transmission may also occur (7).
C. burnetii may cause acute and chronic forms of Q fever in humans, though in many cases infection is asymptomatic and confirmed by serologic diagnosis only (8). The acute form of Q fever manifests usually as a flulike illness or atypical pneumonia, but often it has a protean character with a clinical picture resembling that of nearly any infectious disease (9). Whereas acute Q fever is usually self-limited, chronic Q fever is a serious and often fatal illness with death rates exceeding 65% (10). Illness occurs months to years after the acute infection in 1% to 11% of patients and usually manifests as endocarditis. Infections of arterial aneurysm or prosthesis; bone infection; pseudotumor of the lung; hepatitis; cutaneous, musculoskeletal, or renal involvement; and placentitis in pregnancy with miscarriage are also possible (11).
The first human cases of Q fever in Europe appeared in the Balkans during World War II when strange, febrile, influenzalike infections, named Balkangrippe, were observed among German troops (12,13). Similar infections occurred among allied troops during operations in the Mediterranean area (14,15). In the 1940s, Q fever was recognized in Romania (16), Greece (17), and Bulgaria (18). The Balkans thus became the territory in which C. burnetii could circulate in nature, be transmitted to humans, and be spread to other parts of Europe; for example, Q fever was probably introduced to Slovakia through infected sheep from Romania (6).
Though the first human Q-fever cases in Bulgaria were described as early as 1949 (18), thorough epidemiologic and epizootologic studies started later in connection with the unification of land and livestock farms into state premises and agricultural cooperative units. Concentration of domestic animals (especially cows and sheep) and conditions favoring circulation and maintenance of C. burnetii in nature (ticks, reservoir animals) turned the country into a huge natural focus of Q fever. The occurrence of C. burnetii infection in different parts of the country was 6% to 100% in sheep, 5% to 31% in cattle, and 7% to 34% in goats (19), as confirmed serologically by complement fixation (CF). Infestation of ticks with C. burnetii reached 26% in southwest and 22% in northeast Bulgaria (20).
The situation changed dramatically in the 1990s as the large state premises and cooperative farms collapsed and the number of cows and sheep decreased (e.g., sheep from 8 million in 1990 to 3 million in 1997). As individual farmers started to raise goats for easily accessible food, the number of goats increased from 430,000 in 1990 to more than 1 million in 1997. Moreover, the proportion of sera containing antibodies to C. burnetii from domestic animals from five regions of Bulgaria in 1996 to 1997 also changed; more (90% of 140) samples from goats than from sheep (73% of 118) tested positive. At the same time, the rate of infestation of Dermacentor marginatus, Ixodes ricinus, and Rhipicephalus sanguineus with C. burnetii as demonstrated by the hemocyte test (21) was also very high (25 of 29 ticks tested were infected).
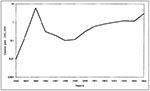
These changes also influenced the occurrence and seasonality of human Q-fever cases in Bulgaria. Until 1990, more than 20 Q-fever outbreaks occurred in several regions of the country, some with hundreds of patients (e.g., 725 cases near Knyezha from 1982 to 1985 [22] and as many as 630 cases in Pavlikeni in 1985 only). These Q-fever epidemics among farmers explain the sharp peak of Q fever incidence in 1985 (Figure 1). A sudden drop and continual decrease thereafter could reflect a return to a nonepidemic situation; the gradual increase in the 1990s was probably associated with an increase in the number of goats (Figure 1). Depicting the seasonality of the disease, the number of goats shifted from winter and spring months (December to May) with a peak in January in the 1980s to spring and summer months (March to August) with a peak in May and June in the 1990s (Figure 2).
Several factors probably contributed to this shift. 1) A change in insemination practices. Until 1990, artificial insemination of ewes was carried out in early autumn, but in the 1990s, this practice was abandoned. 2) Sheep deliver in January and February, whereas goats deliver in March and April. 3) Herds of cattle and flocks of sheep, though concentrated in larger numbers, were separated from most of the population and served as the source of C. burnetii infection usually among farmers and others exposed to animals and their products. 4) An increased number of goats have been kept in very close contact with goat owners and their family members. 5) Goats have been pastured daily (from March until October), so they cross the streets of villages and small towns twice a day. Thus, at present in Bulgaria, goats (rather than sheep or cattle) seem to be an important source of C. burnetii infections for humans. Not only have great numbers of goat owners with their families been exposed to C. burnetii (when tending the goats or consuming their unpasteurized milk products), but also occasional bystanders could contract C. burnetii infection from exposure to the contaminated aerosols created from excrements of the goats, as they repeatedly passed through villages and small towns to their pastures or from exposure to infectious particles generated during parturition or abortion. For example a Q-fever outbreak in Val de Bagnes, Switzerland, which affected 415 persons, occurred 3 weeks after 12 flocks of sheep descended from the Alpine pastures to the valley (8).
The largest Q-fever outbreak was registered in Panagyurische (central part of southern Bulgaria) in the 1990s, after an influenza epidemic (end of 1992, beginning of 1993). From January to June 1993, a second epidemic wave with more than 2,000 cases of an acute flulike respiratory illness and bronchopneumonia occurred. Atypical pneumonia was diagnosed in 589 cases by X-ray examination, and 254 patients were admitted to the regional hospital. Q fever was confirmed serologically only at the end of the epidemic. Of more than 500 persons who recovered from Q-feverlike disease, 60% were seropositive; several laboratories confirmed significant titers (from 80 to 640 in CF and microimmunoflourescence [MIF] tests) of antibodies to phase II C. burnetii. Though most of the patients and those with positive serologic tests were adults 20 to 59 years of age, high positivity was also noticed in children <6 years of age (19%) and in persons 7 to 19 years of age (23%). Most of the patients were not employed in agriculture or the processing of animal products. Serologic examination of domestic animals by CF test gave similar results for goats (26% of 969) and sheep (28% of 421). However, sheep did not seem to serve as a source of C. burnetii infection—they went to pastures far away from the town from February to March. The highest number of human Q-fever cases was observed from April to June when goats delivered their kids and sporadic goat abortions occurred.
A Q-fever outbreak occurred in Panagyurische again in April to June 1995 as evidenced serologically in 78% of 89 patients admitted to the local hospital with bronchopneumonia. Acute Q fever was diagnosed in 28 (31%) on the basis of seroconversion or fourfold rise of antibody titers. The results indicate that Q fever appears to be endemic in the Panagyurische area (with seasonal spring occurrence) and goats are probably the main source of human infection. Nevertheless, such a seasonal Q-fever occurrence has not been restricted to this area of Bulgaria (Table) but occurred in all the regions (Ichtiman and Elin Pelin in the West, Stara Zagora in the South, Blagoyevgrad in the Southwest, Vratza in the Northwest, and Varna in the Northeast) of the country in which it had been followed. Of 252 patients with bronchopneumonia and acute flulike symptoms, 66% (46%-100%) had antibodies to phase II C. burnetii detected by CF or microagglutination (MA) tests. Acute Q fever was confirmed in 73 (29%) patients tested (13% to 60% in different regions). In all these regions, sheep, cattle, and goats have been raised not only in villages surrounding the above-mentioned towns, but also in their suburbs.
Similar results were observed when testing human sera from the serum bank. Of 224 randomly chosen sera collected in nine localities (Gabrovo from the North, Razgrad and Dobrich from the Northeast, Sofia from the West, Blagoyevgrad from the Southwest, and Stara Zagora, Pazardzhik, Haskovo, and Sliven from the South of Bulgaria), 87 (38%) reacted positively with phase II C. burnetii in MA or MIF tests. Serologic positivity varied from 6% in Sliven to 60% in Blagoyevgrad, except for Razgrad, where none were positive (however, only four sera were tested).
Chronic Q-fever cases manifesting as endocarditis were confirmed serologically by high titers from 640 to 1 ml of phase I- and phase II- C. burnetii immunoglobulin (Ig)G antibodies in MIF, by demonstration of specific immunofluorescence in the cuts of aortal valves, and by C. burnetii isolation from the replaced prosthesis in three patients before 1990 (23). Two additional cases of Q-fever endocarditis were diagnosed serologically by MA and MIF tests from 1996 to 1997.
Antibodies to phase II C. burnetii by MA were found in 16 of 18 aborting women with titers of 10 to 320, which indicates the possibility of acute Q-fever infection during pregnancy. In two cases, in paired sera collected in 23-day intervals, a shift from the titer of 160 to seronegativity (titer <10) was observed. Even though abortion tissues were not cultured or tested for C. burnetii, these findings deserve further study, since the possible adverse effects of C. burnetii infection during pregnancy has also been suggested by other authors (24).
In Slovakia, Q fever has been known since 1954 when outbreaks occurred among agricultural workers who contracted the infection from sheep imported from Romania and among workers of a textile plant who were exposed to contaminated imported cotton (6). From that time until the 1980s, the waves of epizootics and small epidemics appeared in factories processing cotton, wool, and hides from Mongolia and China, in a sheep farm with imported breeding rams from England, and in various agricultural premises often connected with excursions of workers to cattle or sheep farms in which C. burnetii infections could have occurred. Veterinary and serologically uncontrolled movement of cattle within the country also contributed to the establishment of domestic coxiellosis (25). Some areas of the southern part of central Slovakia became a natural focus of Q fever, with the D. marginatus tick as the main vector of C. burnetii (6).
Since the 1980s, only sporadic cases of Q fever have been reported from different parts of the country, though almost 3% of approximately 7,000 ticks collected in all districts of Slovakia were found (by the hemocyte test) to harbor C. burnetii, and attempts to recover C. burnetii from pooled positive ticks resulted in the isolation of 10 virulent C. burnetii strains from five ticks, mostly I. ricinus species (26). On the other hand, C. burnetii strains isolated from cow milk were of lower virulence for guinea pigs and mice (Kovácová et al., submitted for publication). Circulation of such low virulent strains among livestock and large-scale vaccination of cattle by inactivated phase I-C. burnetii corpuscular vaccine (one subcutaneous dose consisting of 500 µg of highly purified C. burnetii cells) carried out in the 1970s and 1980s, together with improved veterinary control of domestic animal transport within the country, could explain a decrease in the occurrence of human Q fever in Slovakia. This explanation is supported by results of a serologic survey (carried out from 1989 to 1996) for Q-fever antibodies in groups of farmers or in patients with suspected C. burnetii infection. Of 21,197 human sera tested, 655 (3%) reacted with phase II- C. burnetii antigen in the CF test (until 1992) or (later on) in enzyme-linked immunosorbent assay (ELISA). Acute Q fever (as individual or clustered cases) was diagnosed in 23 sera, not including 113 from the Q-fever epidemic discussed below, on the basis of seroconversion or IgM antibody detection. During the same period, phase-II C. burnetii antibodies were detected in 11% of cattle and in 3% each of sheep and goats.
Improved veterinary control of domestic animal transport within the country, however, cannot exclude the possibility of introducing C. burnetii infection through imported domestic animals or raw materials not tested properly. The use of CF, which is much less sensitive to Q-fever antibodies than other serologic tests (e.g., ELISA [27]), to screen the goats imported to Slovakia from Bulgaria is unsatisfactory, as confirmed in 1993 by the largest reported Q-fever epidemic in Slovakia (28). The epidemic started suddenly during the spring as an outbreak of respiratory infection in inhabitants of a village in West Slovakia. A total of 113 persons were affected from the beginning of March until May 18, as confirmed serologically (seroconversion, detection of IgM antibodies, and high phase-II antibody titers, respectively) by CF, MA, MIF, and ELISA. Of 42 patients admitted to the hospital, 33 had atypical pneumonia (diagnosed by X-ray examination), and 27 had hepatic involvement (diagnosed on the basis of the increased values of liver transaminases). As many as 103 were male patients who used to visit the local pub, in which they contracted infection by the aerosol created from the heavily contaminated garments of boys tending aborting goats. C. burnetii infection in incriminated goats was confirmed serologically (46 of 216 goat sera tested were positive by ELISA) and by seroconversion in mice inoculated with spleen, lung, and liver suspension from an aborted kid.
In contrast to the situation in Bulgaria, a 4-year follow-up of patients from this Q-fever epidemic did not result in clinical or serologic confirmation of any chronic form of the disease (Ková…ová et al., submitted for publication). In addition, evidence of chronic Q fever was obtained neither in the serologic survey carried out in Slovakia from 1989 to 1996, nor in testing of more than 200 patients with chronic cardiovascular disease (some of them exposed to C. burnetii infection through their work). Similarly, observation of patients from other Q-fever epidemics (including those with 98 cases in a cotton-processing plant in nearby Southern Moravia in 1980 [29]) was also negative. Whether this can be explained by C. burnetii strains of different virulence circulating in Bulgaria and Slovakia, respectively, remains to be seen, though in the latest Q-fever epidemic in West Slovakia, Bulgarian C. burnetii strains were presumably involved. However, whereas C. burnetii strains of tick and domestic animals origin isolated in Slovakia may differ, no data are known on the virulence of Bulgarian strains. A total number of human C. burnetii cases can also be important. Whereas in Bulgaria more than 1,000 patients were affected, in Slovakia tens of human cases occurred, so the probability of developing the chronic form of Q fever in Slovakia was lower. The small number of patients in Slovakia could also be explained by earlier diagnosis and proper antibiotic treatment at the early stage of infection. The patients' history, e.g., previous rheumatic disease, should be also taken into consideration.
Epidemiologic and serologic investigations in Bulgaria and Slovakia indicate that an increase in human Q fever in Bulgaria in the 1990s and Slovakia in 1993 was associated with goats. The data on the propensity of goats to transmit C. burnetii to humans from Greece, Cyprus, France, the United States, and even a trans-Pacific cargo ship transporting dairy goats, were summarized by Lang (4). More recently, a cluster of human C. burnetii infections associated with exposure to vaccinated goats and their unpasteurized products was reported from France (30). Goats may pose a threat to human health as a source of C. burnetii infection in every country in which they are raised extensively and are in close contact with humans. However, Q fever can also be contracted from other sources of infection and has been, even in Bulgaria and Slovakia.
Reporting of Q fever in a given territory depends on the attention of public health authorities and the availability of diagnostic methods. Apart from C. burnetii isolation (mainly in cell cultures by a shell-vial method [31] or direct detection, preferably by polymerase chain reaction [32]), these diagnostic methods are based mostly on serologic tests. Sensitivity of serologic tests for screening Q-fever antibodies increased from CF to MA and from MIF to ELISA (27). The cut-off values for individual tests may differ between laboratories and antigens used; for CF and MA tests, 1:8 and 1:16 serum dilutions were acceptable (in Slovakia) and for either test 1:10 serum dilution was acceptable (in Bulgaria). For a more sensitive MIF and ELISA allowing also detection of immunoglobulin classes, diagnostic titers were set at the phase-II IgG > 200 and phase-II IgM > 50 in MIF (33) and at > 128 for the IgM and IgG phase-I responses, but > 512 for the IgM and > 1,024 for the IgG response to phase II C. burnetii in ELISA (34), respectively. Serologic diagnosis of acute Q fever relies on seroconversion from negativity to positivity or at least fourfold rise of phase-II antibodies in paired (acute- and convalescent-phase) serum samples and demonstration of IgM antibody response or high titers (e.g., > 128 in CF and 200 in MIF) of phase-II antibodies in a single serum sample. For diagnosis of chronic Q fever, high titers (i.e., > 200 in CF and > 800 of in MIF) of phase I antibodies, occurring rarely and in low titers in acute Q-fever cases, are required (9).
Q-fever control and prevention measures have been reviewed (35). Apart from the thorough control of imported domestic animals, raw materials, and movement of domestic animals within a country, prevention measures should include adequate disinfection and disposal of animal products of conception and strict hygienic measures in cattle, sheep, and goat farms; plants processing products of these animals; boiling or pasteurization of milk at 62.8°C for 30 minutes or at 71.7°C for 15 seconds; and vaccination. At present, three types of Q-fever vaccine are available for human use: a Formalin-inactivated whole-cell phase-I C. burnetii vaccine used in Australia (36), a chloroform-methanol residue subunit of phase-I C. burnetii recommended by American authors (37), and Q-fever chemovaccine (a soluble subunit vaccine obtained by treatment with trichloroacetic acid of phase-I cells) developed and used in Romania (38) and the former Czechoslovakia (39). For vaccination of domestic animals, corpuscular phase I (in Slovakia) or phase II (e.g., in France) were used. The fact that phase-II vaccine did not protect goats from shedding C. burnetii in milk (30) confirmed that an effective Q-fever vaccine should consist of or be prepared from phase-I C. burnetii (40). Efficient recombinant vaccines, however, should also be pursued.
Mass vaccination of cattle in Slovakia in the 1970s, followed by selective vaccination of cattle in serologically positive herds and elimination of positive reactors in the 1980s could lessen not only distribution of C. burnetii among domestic animals, but also its transmission to humans. However, absence of vaccination of domestic animals in Bulgaria could contribute to the maintenance of C. burnetii and therefore to increased possibility of human infection, though basic natural conditions for circulation of this agent in either country have been similar. Moreover, gradual changes in agriculture in Slovakia during the 1990s resulted in reduced numbers of cattle and sheep but not in the dramatic increase in goat numbers seen in Bulgaria after the collapse of state farms and cooperative units. One can conclude that in Bulgaria there is a permanent threat of more Q-fever outbreaks unless preventive measures, including improvement of veterinary services and vaccination of domestic animals, particularly goats, are established. In Slovakia, because of surveillance, veterinary control, and vaccination of domestic animals, the situation is much better; however, attention should still be paid to avoid introduction of C. burnetii by imported animals and raw materials and the possibility of coxiellosis outbreaks among domestic animals and consequently Q fever in humans.
Dr. Serbezov is consultant at the National Center of Infectious and Parasitic Diseases in Sofia.
References
- Derrick EH. Q fever, a new fever entity: clinical features, diagnosis and laboratory investigation. Med J Aust. 1937;2:281–99.
- Marrie TJ. Epidemiology of Q fever. In: Marrie TJ, editor. Q Fever. Vol 1. The disease. Boca Raton (FL): CRC Press; 1990. p. 49-70.
- Hilbink F, Penrose M, Kovácová E, Kazár J. Q fever is absent from New Zealand. Int J Epidemiol. 1993;22:945–9. DOIPubMedGoogle Scholar
- Lang GH. Coxiellosis (Q fever) in animals. In: Marrie TJ, editor. Vol 1. The disease. Boca Raton (FL): CRC Press; 1990. p. 23-48.
- Sawyer LA, Fishbein DB, McDade JE. Q fever: current concepts. Rev Infect Dis. 1987;9:935–46.PubMedGoogle Scholar
- Rehácek J, Tarasevich IV. Q fever. In: Grešíková M, editor. Acari-borne rickettsiae & rickettsioses in Eurasia. Bratislava: VEDA; 1988. p.203-43.
- Raoult D. Q fever: still a query after all those years. J Med Microbiol. 1996;44:77–8. DOIPubMedGoogle Scholar
- Dupuis G, Petite J, Peter O, Vouilloz M. An important outbreak of human Q fever in a Swiss Alpine Valley. Int J Epidemiol. 1987;16:282–9. DOIPubMedGoogle Scholar
- Kazár J. Q fever. In: Kazár J, Toman R, editors. Rickettsiae and rickettsial diseases. Bratislava: VEDA; 1996. p. 353-62.
- Imhauser K. Viruspneumonien: Q-Fieber und Virusgrippe. Klin Wochenschr. 1949;27:353–60. DOIGoogle Scholar
- Bieling R. Die Balkangrippe das Q Fieber der alten Welt. Beitr Hyg Epidemiol. 1950;:H5.
- Robbins FC, Ragan CA. Q fever in the Mediterranean area: report of its occurrence in allied troops. I. Clinical features of the disease. Am J Hyg. 1946;44:6–22.
- Robbins FC, Gauld RL, Warner FB. Q fever in the Mediterranean area. II. Epidemiology. Am J Hyg. 1946;44:23–50.
- Combiescu D, Vasiliu V, Dumitrescu N. Identification l'une nouvelle rickettsiose chez homme en Roumanie. Comptes Rendus des séances de la Sociéte de biologie Bucharest 1947;141:716-7.
- Caminopetros JP. La Q-fever en Grece: le lait source de l'infection pour l'homme et les animaux. Annals du Parasitologie Paris. 1948;23:107–18.
- Mitov A. Diagnosis of two cases of Q fever in southern Bulgaria. [in Bulgarian]. Bulgarskaja Klinika. 1949;8:610–23.
- Serbezov V, Shishmanov E, Aleksandrov E, Novkirishki V. Rickettsioses in Bulgaria and other Balkan countries. Danov CG, editor. Plovdiv: Christo G. Domov; 1973. p. 223 (in Bulgarian).
- Georgieva G. Ixodid ticks as vectors of rickettsiae in Bulgaria [thesis in Bulgarian]; Sofia, Bulgaria: Military Medical Institute; 1984.
- Rehácek J, Brezina R, Kovacova E, Zupanicicova M. Haemocyte test—an easy, quick and reliable method for the detection of rickettsiae in ticks. Acta Virol. 1971;15:237–40.PubMedGoogle Scholar
- Novkirishki V, Bojadzhian CH, Kijanovska E, Epidemiologic studies of Q fever outbreak in the region of the Knyezha town. [in Bulgarian]. Infektologija. 1994;31:16–9.
- Serbezov V. Q-fever endocarditis: etiology, epidemiology and etiological diagnostics. [in Bulgarian]. Bulgarian Cardiology. 1996;3:36–41.
- Stein A, Raoult D. Q fever and pregnancy in humans and animals. In: Kazár J, Toman R, editors. Rickettsiae and rickettsial diseases. Bratislava: VEDA; 1996. p. 551-7.
- Rehácek J. Epidemiology and significance of Q fever in Czechoslovakia. Zentralblatt für Bakteriologie. Mikrobiologie und Hygiene Series A. 1987;267:16–9.
- Rehácek J, Úrvolgyi J, Kocianová E, Sekeyová Z, Vavreková M, Kovácová E. Extensive examination of different tick species for infestation with Coxiella burnetii in Slovakia. Eur J Epidemiol. 1991;7:299–303. DOIPubMedGoogle Scholar
- Kovácová E, Kazár J, Španìlová D. Analysis of antibody response in humans and goats with the use of different Coxiella burnetii antigenic preparations. In: Kazár J, Toman R, editors. Rickettsiae and rickettsial diseases. Bratislava: VEDA; 1996. p. 463-8.
- Varga V. An explosive outbreak of Q fever in Jedlóvé Kostol'any, Slovakia. Cent Eur J Public Health. 1997;3:180–2.
- Kazár J, Hornícek J, Valihrach J, Krunert Z, Pavlík J, Petrík P, An epidemic of Q fever in a cotton-processing plant. [in Slovak]. Cesk Epidemiol Mikrobiol Imunol. 1982;31:144–51.PubMedGoogle Scholar
- Fishbein DB, Raoult D. A cluster of Coxiella burnetii infections associated with exposure to vaccinated goats and their unpasteurized products. Am J Trop Med Hyg. 1992;47:35–40.PubMedGoogle Scholar
- Musso D, Raoult D. Coxiella burnetii cultures from acute and chronic Q-fever patients. J Clin Microbiol. 1995;33:3129–32.PubMedGoogle Scholar
- Stein A, Raoult D. Detection of Coxiella burnetii by DNA amplification using polymerase chain reaction. J Clin Microbiol. 1992;30:2462–6.PubMedGoogle Scholar
- Tissot Dupont H, Thirion X, Raoult D. Q fever serology: cutoff determination for microimmuno-fluorescence. Clin Diagn Lab Immunol. 1994;1:89–96.PubMedGoogle Scholar
- Waag D, Chulay J, Marrie T, England M, Williams J. Validation of an enzyme immunoassay for serodiagnosis of acute Q fever. Eur J Clin Microbiol Infect Dis. 1995;14:421–7. DOIPubMedGoogle Scholar
- Kazár J, Brezina R. Control of rickettsial diseases. Eur J Epidemiol. 1991;7:282–6. DOIPubMedGoogle Scholar
- Marmion BP, Ormsbee RA, Kyrkou M, Wright J, Worswick DA, Izzo AA, Vaccine prophylaxis of abattoir-associated Q fever: eight years of experience in Australian abattoirs. Epidemiol Infect. 1990;104:275–87. DOIPubMedGoogle Scholar
- Fries LF, Waag DM, Williams JC. Safety and immunogenicity in human volunteers of a chloroform-methanol residue vaccine for Q fever. Infect Immun. 1993;61:1251–8.PubMedGoogle Scholar
- Cracea E, Dumitrescu S, Botez D, Toma E, Bandu C, Sabin S, Immunization in man with a soluble Q fever vaccine. Arch Roum Pathol Exp Microbiol. 1973;32:45–51.PubMedGoogle Scholar
- Brezina R, Schramek Š, Kazár J, Úrvolgyi J. Q fever chemovaccine for human use. Acta Virol. 1974;18:26.
- Kazár J, Rehácek J. Q fever vaccines: present status and application in man. Zentralblatt fur Bakteriologie. Mikrobiologie und Hygiene Series A. 1987;267:74–8.
Figures
Table
Cite This ArticleTable of Contents – Volume 5, Number 3—June 1999
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Ján Kazár, Institute of Preventive and Clinical Medicine, Limbová 14, 833 01 Bratislava, Slovak Republic; fax: 421-737-3906
Top