Volume 7, Number 6—December 2001
Research
Modeling Potential Responses to Smallpox as a Bioterrorist Weapon
Figure 3
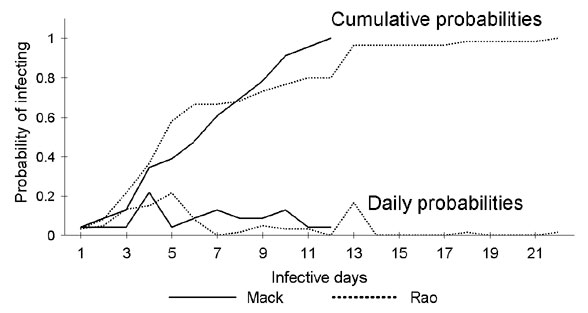
Figure 3. Daily and cumulative probabilities determining when an infectious person infects another person with smallpox (6,19). Day 1 of the infectious period is the first day of the prodromal stage. That is, we have interpreted the source data to reflect the assumption that no spread of infection can occur while an infected person is in the incubating stage.
References
- Henderson DA. The looming threat of bioterrorism. Science. 1999;283:1279–82. DOIPubMedGoogle Scholar
- Henderson DA. Smallpox: clinical and epidemiologic features. Emerg Infect Dis. 1999;5:537–9. DOIPubMedGoogle Scholar
- Bardi J. Aftermath of a hypothetical smallpox disaster. Emerg Infect Dis. 1999;5:547–51. DOIPubMedGoogle Scholar
- Henderson DA, Inglesby TV, Bartlett JG, Ascher MS, Eitzen E, Jahrling PB, Smallpox as a biological weapon: medical and public health management. JAMA. 1999;281:2127–37. DOIPubMedGoogle Scholar
- Rao AR. Smallpox. Bombay: The Kothari Book Depot; 1972.
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. Smallpox and its eradication. Geneva: World Health Organization; 1988.
- Dixon CW. Smallpox. London: Churchill; 1962.
- Anderson RM, May RM. Infectious diseases of humans: dynamics and control. New York: Oxford University Press; 1991.
- Anderson RM, May RM. Population biology of infectious diseases: Part II. Nature. 1979;280:455–61. DOIPubMedGoogle Scholar
- Cliff AD, Haggett P. Statistical modeling of measles and influenza outbreaks. Stat Methods Med Res. 1993;2:43–73. DOIPubMedGoogle Scholar
- Anderson RM, May RM. Population biology of infectious diseases: Part I. Nature. 1979;280:361–7. DOIPubMedGoogle Scholar
- Anderson RM. Transmission dynamics and control of infectious disease agents. In: Anderson RM, May RM, editors. Population biology of infectious diseases. Berlin: Springer-Verlag; 1982. p. 149-77.
- Aron JL, May RM. The population dynamics of malaria. In: Anderson RM, editor. The population dynamics of infectious diseases: theory and application. London: Chapman and Hall; 1982.
- Frauenthal JC. Smallpox: when should routine vaccination be discontinued? The UMAP Expository Monograph Series. Boston: Birkhäuser; 1981.
- Giordano FR, Weir MD, Fox WP. A first course in mathematical modeling. 2nd ed. Pacific Grove (CA): Brooks/Cole Publishing Company; 1997.
- Christie AR. Infectious diseases: Epidemiology and clinical practice. 3rd ed. New York: Churchill Livingstone; 1980.
- Singh S. Some aspects of the epidemiology of smallpox in Nepal. Geneva: World Health Organization (WHO/SE/69.10); 1969.
- U.S. Bureau of the Census. Statistical abstract of the United States: 1999. 119th ed. Washington: Bureau of the Census; 1999.
- Royal Commission on Vaccination. A report on vaccination and its results, based on evidence taken by the Royal Commission during the years 1889-1897. Vol 1. The text of the commission report. London: New Sydenham Society; 1898.
- Smith ADM. Epidemiological patterns in directly transmitted human infections. In: Croll NA, Cross JH, editors. Human ecology and infectious diseases. New York: Academic Press; 1983. p. 333-51.
- Bartlett MS. Measles periodicity and community size. J R Stat Soc [Ser A]. 1957;120:48–60. DOIGoogle Scholar
- Bartlett MS. Critical community size for measles in the United States. J R Stat Soc [Ser A]. 1960;123:37–44. DOIGoogle Scholar
- Arita I, Wickett J, Fenner F. Impact of population density on immunization programmes. J Hyg Camb. 1986;96:459–66. DOIPubMedGoogle Scholar
- Lane JM, Millar JD. Routine childhood vaccination against smallpox reconsidered. N Engl J Med. 1969;281:1220–4. DOIPubMedGoogle Scholar
- Pattanayak S, Sehgal PN, Raghavan NGS. Outbreaks of smallpox during 1968 in some villages of Jaipur district, Rajasthan. Geneva: World Health Organization (WHO/SE/70.20); 1970.
- de Sario V. Field investigation of an outbreak of smallpox at Bawku, Ghana: May-October, 1967. Geneva: World Health Organization (WHO/SE/69.24); 1969.
- Rangaraj AG. An outbreak of smallpox in a village in Afghanistan. Geneva: World Health Organization (WHO/SE/69.9); 1969.
- Glokpor GF, Agle AN. Epidemiological investigations. Smallpox Eradication Programme in Togo: 1969. Geneva: World Health Organization (WHO/SE/70.21); 1970.
- Litvinjenko S, Arsic B, Borjanovic S. Epidemiologic aspects of smallpox in Yugoslavia in 1972. Geneva: World Health Organization (WHO/SE/73.57); 1973.
- de Costa EA, Morris L. Smallpox epidemic in a Brazilian community. Geneva: World Health Organization (WHO/SE/74.64); 1974.
- Presthus GT, Sibiya JB. A persistent focus of smallpox in Botswana. Geneva: World Health Organization (WHO/SE/74.89); 1974.
- Great Britain Ministry of Health. Smallpox, 1961-62. Reports on public health and medical subjects, No. 109. London: Her Majesty's Stationery Office; 1963.
- Evans M, Hastings N, Peacock B. Statistical distributions. 2nd ed. New York: John Wiley & Sons, Inc.; 1993.
- Kaufmann AF, Meltzer MI, Schmid GP. The economic impact of a bioterrorist attack: Are prevention and postattack intervention programs justifiable? Emerg Infect Dis. 1997;3:83–94. DOIPubMedGoogle Scholar
1Others have suggested that the terms "preeruptive" or "initial" are more descriptively accurate of this stage (6). However, because "prodromal" is used in many standard textbooks (7,8,17), we will use this term.
2Prodromal rashes have been recorded, but they were considered to be uncommon occurrences, ". . . not more than 1 in 10." (17).
3The United States stopped routine vaccination of the civilian population in 1972 (5). In July 1998 in the United States, there were approximately 109.9 million persons <30 years of age, representing 41% of the total resident population (20). Most of these people have not been vaccinated against smallpox. In addition, the immunologic status of those who were vaccinated >30 years ago must be considered. Historical data indicate that vaccination 20 to 30 years ago may not protect against infection but will often protect against death (8,21). No reports, however, define the probability of such persons' transmitting the disease to susceptible persons. Faced with such uncertainty, we chose the simplest approach of assuming an unlimited supply of susceptible persons.
4At a 50% daily removal rate, a cohort of all those beginning the first day of overt symptoms is entirely removed in 7 days (8 to 10 days postincubation), with 90% removed in 4 days after they enter the overtly symptomatic period. At a 25% daily removal rate, a cohort is entirely removed 17 days after entering the overtly symptomatic period (18 to 20 days postincubation), with 90% removed in 9 days after entering the overtly symptomatic period. The calculated numbers of those quarantined relate only to those who are infectious (i.e., overtly symptomatic). The model does not take into account those who might also be quarantined along with the infectious persons, such as unvaccinated household contacts and other exposed persons.
5The number, severity, and cost of vaccine-induced side effects is the subject for a separate paper.
6Allowing 3 days for laboratory confirmation assumes that virus loads in clinical specimens may be insufficient to allow use of rapid assays and confirmation must await the results of a culture-based assay, which takes approximately 72 hours. Rapid laboratory confirmation, within 24 hours, is possible.
7Even by reducing transmission from 3 to 2 persons per infectious person and quarantining infectious persons at a rate of 25% per day, the number of new cases at day 365 is 3, not zero (i.e., transmission is not quite completely stopped) (Figure 6). For transmission to cease completely, vaccination must either achieve a 38% reduction in transmission to 1.85 cases per infectious person (assuming a daily quarantine rate of 25%), or quarantine must achieve a 29% daily reduction in the number of infectious persons (assuming vaccination reduces transmission by 33%).
8Although there are some historical data regarding how infected persons interacted and infected others, all such data were collected when circumstances differed from those of today's societies, particularly with regard to travel and spread of information. Although air and other modes of mass travel were common before smallpox was eradicated, the numbers of travelers and the total miles traveled have vastly increased in the past 30 years. Similarly, although mass media were well known and used in the 1960s and 1970s, more outlets are available to spread information than ever before. It is unknown how these and other changes could affect the spread of smallpox.