Volume 22, Number 3—March 2016
Research
Decreased Time to Treatment Initiation for Multidrug-Resistant Tuberculosis Patients after Use of Xpert MTB/RIF Test, Latvia
Figure 3
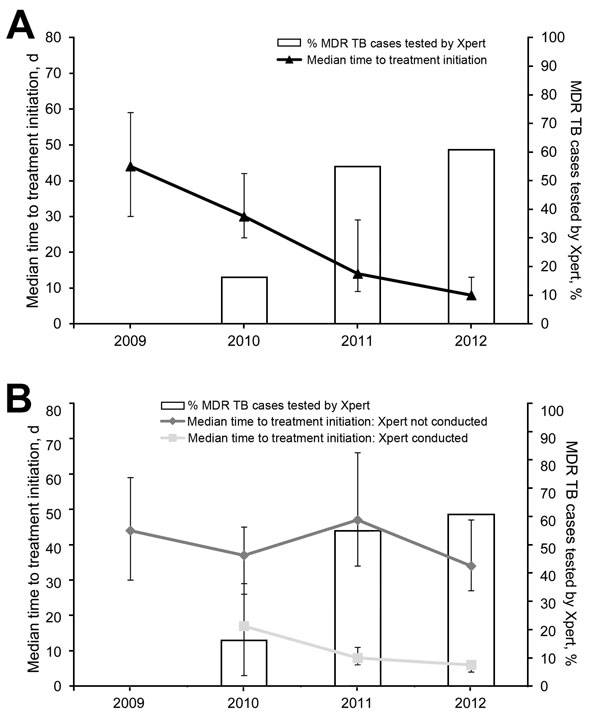
Figure 3. Relationship between use of Xpert MTB/RIF (Xpert) and time to treatment initiation among patients with multidrug-resistant tuberculosis (MDR TB) Latvia, 2009–2012. Shown are percentages of MDR-TB patients that underwent Xpert MTB/RIF testing (bars) and median time to treatment initiation (lines) with binomial distribution–derived CIs (error bars) for A) all patients and B) patients with and without testing by Xpert. MTB, Mycobacterium tuberculosis; RIF, rifampin.
1These authors contributed equally to this article.
Page created: March 01, 2016
Page updated: March 01, 2016
Page reviewed: March 01, 2016
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.