Volume 23, Number 5—May 2017
Research Letter
Carbapenem-Resistant Enterobacter cloacae in Patients from the US Veterans Health Administration, 2006–2015
Cite This Article
Citation for Media
Abstract
We analyzed carbapenem-resistant Enterobacteriaceae (CRE) trends among patients from the US Veterans Health Administration (VHA). After the emergence of CRE in the eastern United States, resistance rates remained stable in Klebsiella pneumoniae but increased in Enterobacter cloacae complex, suggesting a "second epidemic". VHA offers a vantage point for monitoring nationwide CRE trends.
Carbapenem-resistant Enterobacteriaceae (CRE) have become a global public health threat. The epidemic of CRE began in the early 2000s with an outbreak of carbapenem-resistant Klebsiella pneumoniae harboring K. pneumoniae carbapenemase (KPC) in the eastern United States. Since then, KPC-producing K. pneumoniae have emerged in various communities across the country (1). Carbapenem resistance also occurs in other Enterobacteriaceae species and can be mediated by other enzymes, such as OXA-48 and metallo-β-lactamases, especially New Delhi metallo-β-lactamase and Verona integron–encoded metallo-β-lactamase (1). Carbapenem-resistant Escherichia coli occurs infrequently, but recent outbreaks of KPC-producing Enterobacter cloacae raise concerns about the emergence of carbapenem resistance in the E. cloacae complex (1–4).
The Veterans Health Administration (VHA) is the largest integrated healthcare system in the United States. Clinical and microbiologic data for the entire VHA network are accessible through its informatics platforms (5). We used this infrastructure to observe national trends of carbapenem resistance and nonsusceptibility in K. pneumoniae and E. cloacae complex during the past decade.
We identified 224,651 K. pneumoniae and 71,462 E. cloacae complex (E. cloacae, E. asburiae, E. kobei, E. hormaechei, E. xiafangensis) isolates from patients hospitalized during 2006–2015. To minimize bias introduced by variability in susceptiblity reporting, we excluded isolates obtained within 30 days of another isolate from the same patient and isolates from facilities with nonstandard reporting, facilitites that identified <30 isolates in a 2-year period, and facilities that reported carbapenem susceptibilities for <90% of isolates. After these exclusions, 128,431 K. pneumoniae and 38,219 E. cloacae complex isolates from 140 facilities in 40 states, District of Columbia, and Puerto Rico remained for study. We obtained carbapenem (i.e., meropenem, imipenem, ertapenem, doripenem) susceptibility test results (i.e., susceptible, intermediate, or resistant) and calculated rates of resistance and nonsusceptibility to any carbapenem over time, looking at 2-year windows and grouping facilities into 10 regions designated by the US Department of Health and Human Services (https://www.hhs.gov/about/agencies/regional-offices/index.html).
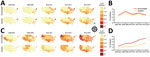
Our data capture the chronologic and geographic spread of carbapenem-resistant K. pneumoniae and E. cloacae complex within VHA (Figure). Before 2010, carbapenem-resistant K. pneumoniae was observed primarily in the eastern United States, but by 2014–2015, the rate of carbapenem resistance detected in K. pneumoniae was >1% in all regions except Regions 8 (South Dakota, North Dakota, Montana, Wyoming, Colorado, Utah) and 10 (Washington, Oregon, Idaho, Alaska). In 2006–2007, carbapenem-resistant E. cloacae complex also had a focus in the East, but in 2008–2009, it was also observed in Region 8. By 2014–2015, carbapenem-resistant E. cloacae complex was centered in the Southwest and Pacific Coast. These regions also had higher rates of carbapenem-nonsusceptible E. cloacae complex, although this phenotype was present in all regions.
The carbapenem-nonsusceptibility rate among K. pneumoniae isolates remained at 3%–4% throughout 2006–2015; however, as with a 2016 study (6), we detected a recent decrease in the rate of carbapenem resistance in K. pneumoniae in Region 2, which includes New York. In contrast, the rates of carbapenem resistance and nonsusceptibility in E. cloacae complex increased nationwide during the last decade, reaching >4% nonsusceptibility and 2.5% resistance in 2014–2015. Also, the proportion of intermediate carbapenem-nonsusceptible isolates was higher for E. cloacae complex (46%) than K. pneumoniae (9%) isolates.
CRE trends during 2006–2015 in the VHA recapitulate the epidemic of carbapenem-resistant K. pneumoniae in the United States and indicate that a “second epidemic” of carbapenem-resistant E. cloacae complex appears to be unfolding. In the United States, the predominant carbapenem-resistant K. pneumoniae genotype is sequence type (ST) 258, which is associated with Tn4401, a mobile genetic element containing blaKPC (7). In contrast, the genetic background of carbapenem-resistant E. cloacae complex is not well defined. Analysis of carbapenem-resistant E. cloacae from the US Midwest and New York, NY, demonstrated dissemination of E. cloacae complex ST171 harboring the blaKPC-3 gene (2,3,8). Further analysis demonstrated that ST171 was associated with a Tn4401 variant within a pBK30683-like plasmid; however, various other plasmids in Enterobacter spp. also harbor blaKPC-3 (4). Of note, in a northeastern US hospital, one third of carbapenem-resistant E. cloacae contained carbapenemases and the rest harbored cephalosporinases, usually only AmpC (9). Nevertheless, we hypothesize that E. cloacae complex contains genotypes with epidemic potential associated with increasing rates of carbapenem resistance observed in the VHA.
The scope of this study did not include molecular characterization, so we could not determine emerging genotypes or detect outbreaks at individual facilities. Also, nonuniform susceptibility testing and interpretation throughout the VHA may affect reporting of CRE. Although criteria for interpretation of carbapenem susceptibility changed during the past decade, the revised breakpoints do not appear to have a major effect on resistance rates in Klebsiella and Enterobacter spp., according to other surveillance data (10). Despite these limitations, the VHA may serve as a vantage point for detecting nationwide trends in antimicrobial drug resistance. Integration of susceptibility testing with molecular characterization at the VHA may help elucidate the changing epidemiology of CRE in the United States.
Dr. Wilson is a researcher at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center in Cleveland, Ohio, USA. Her main research interest is the use of healthcare databases to study infectious diseases in the elderly.
Acknowledgments
This work was approved by the Institutional Review Board at the Louis Stokes Cleveland Department of Veterans Affairs Medical Center.
This work was supported in part by the National Institutes of Health through the Clinical and Translational Science Collaborative of Cleveland (UL1TR000439), National Institute for Allergy and Infectious Disease (R01AI100560, R01AI063517, R21AI114508, and R01AI072219), and VA Research and Development Office (BX001974) and by the VISN 10 Geriatrics Research, Education and Clinical Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
References
- Guh AY, Bulens SN, Mu Y, Jacob JT, Reno J, Scott J, et al. Epidemiology of carbapenem-resistant Enterobacteriaceae in 7 US communities, 2012–2013. JAMA. 2015;314:1479–87. DOIPubMedGoogle Scholar
- Kiedrowski LM, Guerrero DM, Perez F, Viau RA, Rojas LJ, Mojica MF, et al. Carbapenem-resistant Enterobacter cloacae isolates producing KPC-3, North Dakota, USA. Emerg Infect Dis. 2014;20:1583–5. DOIPubMedGoogle Scholar
- Hargreaves ML, Shaw KM, Dobbins G, Snippes Vagnone PM, Harper JE, Boxrud D, et al. Clonal dissemination of Enterobacter cloacae harboring blaKPC-3 in the upper midwestern United States. Antimicrob Agents Chemother. 2015;59:7723–34. DOIPubMedGoogle Scholar
- Chavda KD, Chen L, Fouts DE, Sutton G, Brinkac L, Jenkins SG, et al. Comprehensive genome analysis of carbapenemase-producing Enterobacter spp.: new insights into phylogeny, population structure, and resistance mechanisms. MBio. 2016;7:e02093–16. DOIPubMedGoogle Scholar
- US Department of Veterans Affairs. Health Services Research and Development. VA Informatics and Computing Infrastructure (VINCI) [cited 2016 Sep 8]. http://www.hsrd.research.va.gov/for_researchers/vinci/
- Park SO, Liu J, Furuya EY, Larson EL. Carbapenem-resistant Klebsiella pneumoniae infection in three New York City hospitals trended downwards from 2006 to 2014. Open Forum Infect Dis. 2016;3:ofw222. DOIPubMedGoogle Scholar
- van Duin D, Perez F, Rudin SD, Cober E, Hanrahan J, Ziegler J, et al. Surveillance of carbapenem-resistant Klebsiella pneumoniae: tracking molecular epidemiology and outcomes through a regional network. Antimicrob Agents Chemother. 2014;58:4035–41. DOIPubMedGoogle Scholar
- Gomez-Simmonds A, Hu Y, Sullivan SB, Wang Z, Whittier S, Uhlemann AC. Evidence from a New York City hospital of rising incidence of genetically diverse carbapenem-resistant Enterobacter cloacae and dominance of ST171, 2007-14. J Antimicrob Chemother. 2016;71:2351–3. DOIPubMedGoogle Scholar
- Pecora ND, Li N, Allard M, Li C, Albano E, Delaney M, et al. Genomically informed surveillance for carbapenem-resistant Enterobacteriaceae in a health care system. MBio. 2015;6:e01030–15. DOIPubMedGoogle Scholar
- Rennie RP, Jones RN. Effects of breakpoint changes on carbapenem susceptibility rates of Enterobacteriaceae: Results from the SENTRY Antimicrobial Surveillance Program, United States, 2008 to 2012. Can J Infect Dis Med Microbiol. 2014;25:285–7. DOIPubMedGoogle Scholar
Figure
Cite This ArticleTable of Contents – Volume 23, Number 5—May 2017
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Federico Perez or Robert A. Bonomo, Louis Stokes Cleveland Department of Veterans Affairs Medical Center; 10701 East Blvd, Cleveland, OH 44106, USA; or
Top