Volume 27, Number 8—August 2021
Research Letter
Tuberculosis-Associated Hospitalizations and Deaths after COVID-19 Shelter-In-Place, San Francisco, California, USA
Cite This Article
Citation for Media
Abstract
A mandated shelter-in-place and other restrictions associated with the coronavirus disease pandemic precipitated a decline in tuberculosis diagnoses in San Francisco, California, USA. Several months into the pandemic, severe illness resulting in hospitalization or death increased compared with prepandemic levels, warranting heightened vigilance for tuberculosis in at-risk populations.
Since the emergence of a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease (COVID-19), unprecedented measures have been recommended to reduce transmission. In San Francisco, California, USA, progressively restrictive health officer orders implemented since early 2020 have included travel quarantines, shelter-in-place (SIP), deferral of routine medical appointments and elective surgeries, closure of public-facing events and businesses, and isolation and quarantine when appropriate (1). Nationwide, disruptions in medical services have contributed to delaying or avoiding routine care and a decrease in non–COVID-19-related hospital admissions and emergency department visits (2). Similarly, worldwide tuberculosis (TB) case reports have declined, including in San Francisco, where a ≈60% decrease in newly diagnosed TB cases compared with prior years was observed in the first 4 months of the pandemic (3,4).
The San Francisco Department of Public Health (SFDPH) Tuberculosis Prevention and Control Program manages all cases of active TB in San Francisco residents (≈881,549 population). In 2019, San Francisco had a high incidence of TB, with rates >4-fold higher (11.9 cases/100,000 persons) than the national rate. The affected population is predominantly non–US-born (86%) with >80% residing in the United States >5 years (5). We reviewed overall numbers of active TB case-patients in San Francisco and newly diagnosed cases including those resulting in hospitalization, intensive care unit admission, and death. We divided our analysis into 2 periods: pre-SIP (January 1, 2019–March 15, 2020) and during SIP (March 16, 2020–January 31, 2021). TB was reportable within 1 working day of diagnosis. Cases were diagnosed by microbiologic testing or medical assessment for consistent clinical and radiographic findings. All patients who received a TB diagnosis after SIP began were tested for SARS-CoV-2 co-infection at the time of TB diagnosis, except for 7 patients during March–May 2020, when testing was less available. For all fatalities, we used a standardized algorithm to review medical records and death certificates to determine whether cause of death was TB-related. Because these activities were public health surveillance and not research, review by institutional review board was not requested.
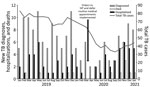
During the 14.5-month pre-SIP period, the monthly average number of patients receiving TB treatment was 73.0 persons, compared with 42.7 persons during the 10.5-month SIP period, resulting in a 42% reduction. The initial SIP period was marked by low numbers of new TB diagnoses during mid-March through June; increasing numbers starting in July, when more case-patients had TB diagnosed while they were hospitalized or dying from TB (Figure). Pre-SIP, a total of 114 patients (average 7.9 patients/month) were newly diagnosed with TB. A total of 38 (33.3%) patients were hospitalized, including 5 (4.4%) who required intensive care. A total of 4 (3.5%) patients died with cause of death assessed as TB-related. In comparison, after SIP began, 52 patients (average 5.0 patients/month) were newly diagnosed with TB. A total of 33 (63.5%) patients were hospitalized, including 12 (23.1%) patients who required intensive care; 7 (13.5%) patients died with cause of death assessed as TB-related. No patients diagnosed with TB during SIP reported having previous SARS-CoV-2 infection; all patients screened for SARS-CoV-2 had negative results. One patient experienced new-onset low-grade fever and cough 37 days after starting TB treatment and subsequently tested SARS-CoV-2 positive; this patient had no new radiographic abnormalities or COVID-19–related complications. More patients during SIP than before SIP required hospitalization, received intensive care, or had a TB-related death (p<0.05 by Pearson χ2 test (Table). We found no difference in duration of TB symptoms pre-SIP (median 1 month, range 0–120 months) than that during SIP (median 1.5 months, range 0–24 months).
Our preliminary findings suggest that delayed TB diagnosis early in the pandemic, coinciding with implementation of SIP and other restrictive measures, might have contributed to an increasing proportion of patients who later experienced severe illness or death. Although we used SIP as a proxy, other factors probably contributed to the trend. The same racial, ethnic, and socioeconomic inequities that contributed to limited healthcare access during the COVID-19 pandemic are prevalent in TB-infected populations (6). Symptomatic patients might have been reluctant or unable to seek medical evaluation, thereby leading to worsening TB disease. The overlap of signs, symptoms, and abnormal radiographic findings for COVID-19 and TB could have resulted in prioritizing COVID-19 screening over TB diagnosis.
Our observations are a snapshot in time and are not representative of TB activity in other cities or regions where COVID-19 transmission rates and corresponding SIP and public health responses differ. Nevertheless, we collected real-world data consistent with the Stop-TB Partnership modeling studies predicting that prolonged disruption of TB activities could result in an excess of millions of TB cases and deaths through 2025 (7). As vaccination rates increase and restrictions ease, continued vigilance and public messaging about the importance of early diagnosis of TB in high-risk populations remain critical.
Dr. Louie is the medical director of the San Francisco Department of Public Health’s Tuberculosis Prevention and Control Program. Her research interests include the epidemiology, clinical management, and treatment of tuberculosis in older populations.
Acknowledgment
We thank the SFDPH Tuberculosis clinic staff for their dedicated care during the COVID-19 pandemic, with special acknowledgement to Eva Cheung, Sheila Davis-Jackson, Rita Estrada, Michelle Huang, Ana Li, George Lee, Talibah Miller, Luc Marzano, Min Naing Ma Khine, Allison Philips, Manuel Penton, Cathleen Qing, Lin Qiu, Jennifer Stella, and Pubu Zhuoga. We also thank Chris Keh for her review and helpful comments on our manuscript.
References
- San Francisco Department of Public Health. Coronavirus (COVID-19) health orders [cited 2021 Mar 22]. https://www.sfdph.org/dph/alerts/coronavirus-healthorders.asp
- Czeisler ME, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–7. DOIPubMedGoogle Scholar
- World Health Organization. Global tuberculosis report 2020 [cited 2021 Mar 22]. https://apps.who.int/iris/bitstream/handle/10665/336069/9789240013131-eng.pdf
- Louie JK, Reid M, Stella J, Agraz-Lara R, Graves S, Chen L, et al. A decrease in tuberculosis evaluations and diagnoses during the COVID-19 pandemic. Int J Tuberc Lung Dis. 2020;24:860–2. DOIPubMedGoogle Scholar
- California Department of Public Health Tuberculosis Control Branch. Tuberculosis disease data and publications [cited 2021 Mar 22]. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/TB-Disease-Data.aspx
- Anderson KE, McGinty EE, Presskreischer R, Barry CL. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4:
e2034882 . DOIPubMedGoogle Scholar - Stop TB. Partnership. The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modeling analysis [cited 2021 Mar 22]. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf
Figure
Table
Cite This ArticleOriginal Publication Date: June 11, 2021
1These senior authors contributed equally to this article.
Table of Contents – Volume 27, Number 8—August 2021
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Janice Louie, San Francisco Department of Public Health Tuberculosis Prevention and Control Program, 2460 22nd St, Bldg 90, 4th Fl, San Francisco, CA 94110, USA
Top