Volume 29, Number 6—June 2023
Research
SARS-CoV-2 Vaccine Effectiveness against Omicron Variant in Infection-Naive Population, Australia, 2022
Abstract
SARS-CoV-2 transmission in Western Australia, Australia, was negligible until a wave of Omicron variant infections emerged in February 2022, when >90% of adults had been vaccinated. This unique pandemic experience enabled assessment of SARS-CoV-2 vaccine effectiveness (VE) without potential interference from background immunity from prior infection. We matched 188,950 persons who had a positive PCR test result during February–May 2022 to negative controls by age, week of test, and other possible confounders. Overall, 3-dose VE was 42.0% against infection and 81.7% against hospitalization or death. A primary series of 2 viral-vectored vaccines followed by an mRNA booster provided significantly longer protection against infection >60 days after vaccination than a 3-dose series of mRNA vaccine. In a population free from non–vaccine-derived background immunity, vaccines against the ancestral spike protein were ≈80% effective for preventing serious outcomes from infection with the SARS-CoV-2 Omicron variant.
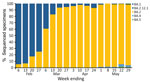
Until February 2022, Western Australia (WA), Australia, successfully delayed sustained transmission of SARS-CoV-2 by using rigorous international quarantine and state border entry restrictions, supported by comprehensive local outbreak control measures when breaches occurred. Data corroborating no substantive community transmission of SARS-CoV-2 in WA until February 2022 include the incidence of reported laboratory-confirmed SARS-CoV-2 infections (Figure 1) and serologic testing of blood donors. By the time WA lifted restrictions and experienced the first wave of SARS-CoV-2 infection, >90% of the state’s residents >16 years of age had received >2 doses of a SARS-CoV-2 vaccine (1). The WA public health laboratory, PathWest Laboratory, determined which SARS-CoV-2 variants were circulating in the state during the first pandemic wave. During the study period (February 1–May 31, 2022), all 2,695 specimens for which lineage could be assigned were the Omicron variant, of which 2,668 (99%) were designated as BA.1 or BA.2 sublineage (Figure 2).
This unique pandemic experience enabled real-world assessment of vaccine effectiveness (VE) without potential bias caused by population-level background immunity resulting from prior infection. With this study, we assessed VE for mRNA vaccines and viral-vectored SARS-CoV-2 vaccines against laboratory-confirmed infection and severe illness caused exclusively by the Omicron variant in a SARS-CoV-2–naive population. This work was approved by the WA Department of Health Human Research Ethics Committee (RGS0000005522).
Study Design
We used a test-negative case–control design to compare persons >16 years of age who had positive PCR SARS-CoV-2 test results with matched controls who were SARS-CoV-2 negative. We compared the odds of vaccination among those with PCR-confirmed SARS-CoV-2 infection or severe COVID-19 with the odds of vaccination among matched PCR-confirmed negative controls.
Data Linkage
In early 2020, WA created a statewide linked data repository to collect information essential for public health management of the pandemic, including SARS-CoV-2 vaccinations that began in February 2021 (2). In brief, COVID-19 vaccination data from the Australian Immunisation Register (AIR; Appendix) were linked to existing WA Department of Health data collections, including statewide hospital admission data, mortality data, and SARS-CoV-2 pathology test results.
Ascertainment of Infection
All persons with >1 SARS-CoV-2 PCR tests performed within the study period were eligible for inclusion. We included in the analysis only a person’s first positive or negative PCR test result during the study period. Persons who initially tested negative but subsequently tested positive during the study period were removed from the negative test pool and reclassified as a case-patient (i.e., each person appeared once in the dataset, as either a case-patient or a control). Because the reason for SARS-CoV-2 testing was not recorded in the data repository, we excluded persons with >20 test results reported during January 2020–May 2022 because those persons were probably subjected to regular asymptomatic screening for employment purposes. We also excluded persons with only SARS-CoV-2 rapid antigen test (RAT) results because negative RAT results were not required to be reported and compliance with mandatory reporting of positive RAT results is unknown.
Vaccination Data
For this analysis, we established vaccination status at the time of the person’s eligible SARS-CoV-2 PCR test result by linking the person to their respective SARS-CoV-2 immunization history in AIR. We included in our analysis persons who received any dose of vaccine >14 days before the eligible PCR result and excluded persons who had received a vaccine dose <14 days before the eligible PCR result. We defined unvaccinated persons as those who had no record of receiving a SARS-CoV-2 vaccine dose before their linked PCR test result.
The vaccines analyzed were the adenovirus-vectored vaccine produced by AstraZeneca (ChAdOx1, https://www.astrazeneca.com) and the mRNA vaccines produced by Pfizer-BioNTech (BNT162b2, https://www.pfizer.com) and Moderna (mRNA-1273, https://www.modernatx.com). We defined a homologous 3-dose vaccination schedule as 2 doses of an mRNA vaccine and an mRNA booster dose, regardless of brand/manufacturer, and a heterologous 3-dose vaccination schedule as 2 doses of ChAdOx1 followed by an mRNA booster dose, regardless of brand/manufacturer. Matched pairs in which the case-patient or control had received a protein-based SARS-CoV-2 vaccine, a ChAdOx1 booster dose, or a mixed 2-dose primary schedule (ChAdOx1 and an mRNA vaccine) were few; we excluded those pairs from subanalysis examining heterologous and homologous vaccine combinations.
Hospitalization and Mortality Data
During the study period, we extracted data from the WA Hospital Morbidity Data Collection (3) and linked them to all SARS-CoV-2 test results for specimens collected. We defined a SARS-CoV-2 hospitalization as >1 inpatient admissions 0–7 days after the date of a positive PCR result. To reduce potential bias that might be introduced through routine preadmission SARS-CoV-2 screening, we excluded admissions for patients indicated by the specialty of the admitting clinician to be unlikely to have been hospitalized for treatment of COVID-19 and for patients admitted for boarding purposes (Table 1). We also performed supplementary sensitivity analyses, which included all hospital admissions regardless of admitting clinician specialty or those defined as a COVID-19 hospitalization on the basis of select codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM).
The WA Registry of Births, Deaths and Marriages (https://www.wa.gov.au), the mandatory repository for death reports in WA, provided mortality data. We defined SARS-CoV-2–associated deaths as death from any cause 0–30 days after an eligible PCR test and included those cases in the analysis. We defined severe disease as SARS-CoV-2 hospitalization, an associated death, or both.
To identify pre-existing medical conditions that could potentially increase a person’s risk for SARS-CoV-2 infection or severe disease, we reviewed any hospital admissions in the 24 months before their eligible PCR test. We selected 14 diagnostic categories and the ICD-10-AM codes used to define them, based on previous literature (Table 2) (4). If a person had any of the ICD-10-AM codes listed as either a principal or secondary diagnosis for an admission in the 24 months before their eligible PCR test, they were assigned a score of 1 for the corresponding diagnostic category. We then summed the total number of unique diagnostic categories assigned a score of 1 for each person, yielding a score of 0–14 (0 if there had been no admissions or only admissions that did not include any of the selected ICD-10-AM codes). We used this aggregate comorbidity score as a proxy index of underlying conditions and controlled for it in the analyses.
Statistical Analyses
We assessed VE by using conditional logistic regression of matched case–control pairs. We calculated adjusted odds ratios (aORs) by using the clogistic function in the Epi package in R version 4.1.0 (The R Foundation for Statistical Computing, https://www.r-project.org). Vaccine effectiveness was defined as (1 – aOR) × 100 and is presented with 95% CIs. We assessed differences between odds ratios by calculating the absolute difference between the log odds and the SEs of the difference. We calculated p values by using z-scores; to account for multiple testing, we considered p<0.01 significant.
Case-patients and controls were matched on week of eligible PCR test, age group (16–19 years, then 10-year intervals thereafter), sex, Aboriginality (defined as Aboriginal and/or Torres Strait Islander ancestry), Index of Relative Socioeconomic Advantage and Disadvantage decile (5) (a score of 1 demonstrating relatively greater disadvantage and a score of 10 indicating a relative lack of disadvantage), and comorbidity score using by the MatchIt package (6) on a 1:1 basis. We randomly sorted all eligible case-patients and controls by using the sample function before matching.
We calculated effectiveness by comparing unvaccinated persons with those who had received either 2 or 3 doses of vaccine. We also performed subanalyses to examine VE for breakthrough infection by time since last vaccine dose and between the homologous and heterologous 3-dose vaccination schedule. Analysis of VE against severe disease included positive case-patients (by PCR) with severe disease who, along with their matched controls, received 2 or 3 vaccine doses.
A total of 1,306,453 PCR tests were reported for specimens collected during February 1, 2022–May 31, 2022, from which 188,950 positive case-patients and 188,950 negative matched controls were eligible for inclusion in the analysis (Table 3; Figure 3). Of the 377,900 study participants, 30,420 (8%) were unvaccinated at the time of testing, 84,237 (22%) had received 2 doses, and 263,243 (70%) had received 3 doses.
VE against Breakthrough Infection of Any Severity
Overall, in adjusted analyses comparing those who were unvaccinated with those who had received 2 vaccine doses, VE for preventing PCR-confirmed infection of any severity was 24.9% (95% CI 21.2%–28.4%), increasing to 42.0% (95% CI 40.2%–43.6%) for persons who had received 3 doses (Table 4). Breakthrough infection of any severity waned notably after a booster dose. For those who had received a booster dose 15–29 days before testing, VE was 70.7% (95% CI 67.4%–73.7%) but fell to 13.5% (95% CI 5.6%–20.8%) for those whose booster was administered >120 days before testing (Figure 4). The median time between the most recent vaccine dose and PCR test date was 21 days longer for persons who received 2 doses (101 days) than for those who received 3 doses (80 days); given the waning immunity after 3 doses, it is possible that increased time since vaccination contributed to lower VE estimates for 2 versus 3 doses.
VE against Severe Disease
Hospitalizations and deaths in the study cohort were rare. Among the 188,950 matched case-patients, there were 264 deaths within 30 days of testing and 1,456 hospital admissions within 7 days, excluding persons admitted under clinician specialties (Table 1).
Overall, VE against severe disease for 2 doses of vaccine was 41.9% (95% CI 4.8%–64.5%) and increased to 81.7% (95% CI 73.9%–87.2%) for 3 doses (Table 5). The number of case-patients with severe disease in individual time strata was insufficient to permit meaningful VE estimates to be generated by time since last vaccination.
VE for Homologous versus Heterologous 3-Dose Series
Our analysis of VE by different vaccine series was restricted to 100,142 case-patients who received either a homologous or heterologous series of 3-dose vaccination (Table 6), as defined previously, and their matched controls. Persons who were vaccinated according to the heterologous versus homologous schedule were older (median age at test 65 vs. 38 years), more likely to be male, and more likely to have >1 comorbidity (Table 7).
VE was higher, although not significantly, up to 60 days after administration of the booster dose among persons who received the homologous or heterologous 3-dose vaccination series. However, VE was significantly higher among those who received a heterologous 3-dose vaccination series 60 days through <120 days of follow-up (Figure 5).
Restricting the samples to those <60 years of age to account for differences in behavior that may contribute to differential breakthrough infection rates yielded similar results. We observed the same pattern of waning immunity in the homologous and the heterologous groups, and protection was significantly higher from 60 to <120 days of follow-up (data not shown) for those on the heterologous schedule
Consistent with the results for breakthrough infection, VE against severe disease was ≈10% higher for those on the heterologous schedule (85.7%, 95% CI 73.1%–92.4%) than on the homologous mRNA schedule (75.8%, 95% CI 61.5%–84.8%), although that difference was not statistically significant in the context of a relatively small number of severe outcomes (p = 0.19). Low numbers of severe outcomes also precluded further analysis of effectiveness by time since vaccination.
Sensitivity Analyses
We performed sensitivity analyses to explore the potential effects of measurement bias, including the effect of using different options for defining disease severity and selecting covariates for matching case-patients to controls. We found no statistically significant effect on VE for severe disease when we restricted hospitalizations to those likely to be for COVID-19 by selecting specific ICD-10-AM codes used for the primary diagnosis instead of the specialty of the admitting clinician (point estimates for VE after 3 doses changed from 79.2% when restricted by primary diagnosis codes to 81.7% when restricted by admitting clinician specialty). In addition, we explored using different time frames to capture hospitalizations after a positive PCR, specifically 0–14, 2–14, and 2–9 days. VE estimates for severe disease did not differ significantly when we varied the window for hospitalization from 0–7 days to these alternate time frames.
Last, we re-ran the analyses while individually and sequentially adding covariates of interest to the matching algorithm to explore potential effects of confounding. Matching by age group and week of PCR test was sufficient to produce stable VE estimates that were statistically similar to those observed when matching on the full set of covariates for infection of any severity and severe disease.
The ability of WA to limit the introduction of SARS-CoV-2 and prevent sustained local transmission 2 years into the pandemic provides a rare opportunity to assess VE in a population without potential confounding from prior asymptomatic or undiagnosed infection, factors that could affect VE assessments performed in almost all other settings. An assessment of VE in Sydney, New South Wales, Australia, also cited low rates of SARS-CoV-2 background infections in its study population, but WA and metropolitan Sydney have had different pandemic experiences (4). Cohort follow-up for the New South Wales study began in January 2022, by which time 157,880 SARS-CoV-2 infections had been reported in the Sydney metropolitan area, largely the result of a protracted outbreak of the Delta variant in 2021 (7). Given that an estimated 40% of all SARS-CoV-2 infections are thought to be asymptomatic (8) and that the degree of underascertainment of those with mild illness who do not seek testing is unknown, it is difficult to quantify with certainty the extent of prior SARS-CoV-2 infection in the Sydney cohort. In contrast, the very low number of locally acquired infections identified before mid-February 2022 in WA (in the context of high rates of testing and robust contact tracing) and the extremely low rate of nucleocapsid antibody positivity among WA blood donor specimens collected during late February–early March 2022 (9) provide convincing evidence that prior SARS-CoV-2 infection was close to negligible among the population used for our analysis.
Most of our key findings are consistent with those from previous studies (10–12). First, overall VE against breakthrough infection of any severity across the full study period for persons who received 2 doses of vaccine was low (24.9% vs. 42.0% for those who received 3 doses). Subanalyses demonstrated that for those who received a booster dose, VE against any infection was near 71% at 15–29 days after vaccination but declined to <14% by 120 days.
Second, protection against severe disease after 3 vaccine doses was much higher than that after 2 doses; overall VE was estimated to be >80%. This finding is relevant because there has been concern that the level of protection afforded by vaccines based on the spike protein of the ancestral strain would be inadequate against Omicron variants, necessitating development of new bivalent vaccines designed to enhance the immune response to Omicron-specific epitopes (10).
This study showed considerable protection from monovalent vaccines against clinically severe illness during an exclusively Omicron wave among a population with negligible background immunity from exposure to the ancestral lineage or previous variants of concern. Our study definitively demonstrates that ancestral strain vaccines still provide substantial protection against severe disease caused by newer variants among a population free from potential confounding of previous immunity conferred by natural infection with an earlier variant.
Vaccine-derived cross-protection observed in our setting may have implications for SARS-CoV-2 vaccine science going forward, specifically for assessing the need to continually design new variant-specific vaccines as the virus evolves. Although greater follow-up time is needed, these data support the hypothesis that vaccine effectiveness against severe disease caused by Omicron is likely to be substantially higher than the estimates against symptomatic disease, as has been observed for previous variants of concern (13–15).
We observed that a heterologous schedule consisting of 2 primary doses of ChAdOx1 followed by a booster dose of an mRNA vaccine provided significantly greater protection against infection >60 days after the last dose, compared with a homologous 3-dose series of mRNA-based vaccines (mostly 3 doses of BNT162b2). This finding is unlikely to be explained by recipients of the heterologous vaccine schedule being inherently less prone to COVID-19 because after the association between ChAdOx1 and thrombotic events was identified, ChAdOx1 was almost entirely administered to persons >60 years of age across Australia. However, in accordance with guidance in Australia about brand-based differences for recommended first- and second-dose intervals, the median time between 2 doses of an mRNA primary series in our cohort was 27 days; for a ChAdOx1 primary series, it was 84 days. It is therefore possible that the longer interval between doses contributed to the more durable protection we observed with the heterologous schedule.
A study of Omicron infections in England found that VE against symptomatic illness was similar between those who received 2 doses of either ChAdOx1 or BNT162b2 followed by a booster dose of BNT162b2, specifically 62.4% and 67.2% given 2–4 weeks after the booster, falling to 39.6% and 45.7%, respectively, after >10 weeks (10). One key difference between our setting and that of the study in England is that in late 2020, the United Kingdom began recommending up to 12 weeks between the first and second doses of BNT162b2, a practice uncommon in the WA cohort, and a longer interval between BNT162b2 doses has been shown to enhance immunogenicity (13).
Alternatively, the superior performance of the heterologous schedule in protecting against Omicron infection in WA may be a real phenomenon, unmasked without interference from substantial levels of background immunity caused by prior infections with earlier variants. The enhanced immune response, and in some instances clinical protection against non-Omicron variants, produced by heterologous vaccination schedules has been documented in a variety of settings (14,15).
Among the limitations of our study, our analysis was restricted to using PCR test results from licensed laboratories to determine a person’s status as a case-patient or control and excluded self-administered RATs reported by the general public. This approach was necessary because RAT results were not systematically linked to other datasets used in this analysis. However, even if possible, including RAT results in our setting would have been methodically undesirable because reporting of negative RAT results is not mandatory and the degree of underreporting of positive RAT results by the public is not quantifiable. Furthermore, because there may be relevant differences between those who seek PCR testing and those who choose to self-administer a RAT, including only positive RAT results would have the potential to introduce significant bias when using a VE study design that explicitly relies on matching test-positive case-patients to similar test-negative controls.
Another limitation is that although we attempted to control for relevant confounders, we were limited by the information available in the data repository, and the potential for residual confounding remains. For example, without knowing the reasons for obtaining a PCR test, we could not exclude tests performed for asymptomatic screening, perhaps before an elective hospital admission or for work requirements. Instead, to account for this limitation, we created a surrogate by excluding all tests for persons with >20 tests over the study period and admissions to hospital services not likely to be treating COVID-19. Likewise, because we were not able to directly access information about a person’s comorbidities, we created a comorbidity score based on hospital ICD-10-AM codes accumulated in the previous 2 years. Although we believe those strategies reduced confounding, they are probably imperfect proxies.
Among the strengths of this study, first, the entire cohort of persons >16 years of age who were tested for SARS-CoV-2 by PCR was eligible for inclusion, which resulted in a large sample, probably representative of the population at risk during the study period. Second, we accessed all SARS-CoV-2 PCR results from every private and public clinical laboratory in the state notified to the WA Department of Health as required by law. Third, we used a comprehensive linked data collection, which included hospitalization data from public and private hospitals and mortality data for the entire state. Fourth, vaccination status was obtained from a population-based, whole-of-life, mandatory national immunization register. AIR data are generally considered to be of good quality (16), and there was a strong incentive for persons to be sure that their COVID-19 vaccination record was accurate and up to date because activities such as employment and attending public venues were dependent on vaccination status (17). Last, the pandemic experience in WA enabled assessment of VE in a SARS-CoV-2 infection–naive cohort, which eliminated potential interference from non–vaccine-derived prior immunity.
In summary, as a result of a sustained, concerted effort to prevent introduction and spread of SARS-CoV-2 during the first 2 years of the pandemic, WA was in a unique position to evaluate, on the basis of the ancestral spike protein, the effectiveness of vaccines to prevent infection and severe disease caused by the Omicron variant in a population that had not experienced prior local SARS-CoV-2 transmission. We demonstrated that VE against infection of any severity was ≈70% up to 1 month after vaccination but waned to very low levels by 4 months. Compared with a homologous 3-dose mRNA vaccine series, a heterologous series consisting of 2 doses of ChAdOx1 followed by an mRNA booster provided significantly longer protection after 60 days, up to 4 months. Protection against hospitalization and death after 3 doses was high (i.e., ≈80%), reinforcing the value of SARS-CoV-2 vaccines for preventing serious outcomes from SARS-CoV-2 infection.
Dr. Bloomfield is a communicable disease epidemiologist with the Immunisation Program in the WA Department of Health, and a senior lecturer for Population and Preventive Health, School of Medicine (Fremantle), University of Notre Dame Australia. Her research interests are vaccine preventable diseases, vaccine safety and effectiveness, nosocomial infections, and antimicrobial resistance.
Acknowledgment
We thank Paul Knight and Dylan Barth for providing SARS-CoV-2 testing and case data (Figure 1). We also thank Chisha Sikazwe, Avram Levy, and staff within the Microbial Surveillance unit at PathWest Laboratory Medicine, Perth, Western Australia, for providing lineage data (Figure 2). Last, we thank the staff at the Western Australian Data Linkage Branch, Death Registrations, COVID-19 Pathology Data Collection, Hospital Morbidity Data Collection, and AIR for providing linked health data.
References
- Australian Government. COVID-19 vaccine roll-out: 01 February 2022 [cited 2023 Jan 30]. https://www.health.gov.au/sites/default/files/documents/2022/02/covid-19-vaccine-rollout-update-1-february-2022.pdf
- Eitelhuber T, Ngeh S, Bloomfield L, Chandaria B, Effler P. Using data linkage to monitor COVID-19 vaccination: development of a vaccination linked data repository. Int J Popul Data Sci. 2022;5:5. DOIGoogle Scholar
- Government of Western Australia Department of Health. Hospital morbidity data collection: data specifications [cited 2023 Jan 30]. https://www.health.wa.gov.au/-/media/Corp/Policy-Frameworks/Information-Management/Patient%20Activity%20Data/Supporting/Hospital-Morbidity-Data-Collection-Data-Specifications-2022.pdf
- Liu B, Gidding H, Stepien S, Cretikos M, Macartney K. Relative effectiveness of COVID-19 vaccination with 3 compared to 2 doses against SARS-CoV-2 B.1.1.529 (Omicron) among an Australian population with low prior rates of SARS-CoV-2 infection. Vaccine. 2022;40:6288–94. DOIPubMedGoogle Scholar
- Australian Bureau of Statistics. 2033.0.55.001—Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016 [cited 2023 Jan 30]. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016?OpenDocument
- Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42:1–28. DOIGoogle Scholar
- Government NSW. COVID-19 cases data [cited 2023 Jan 30]. https://data.nsw.gov.au/nsw-covid-19-data/cases
- Ma Q, Liu J, Liu Q, Kang L, Liu R, Jing W, et al. Global percentage of asymptomatic SARS-CoV-2 infections among the tested population and individuals with confirmed COVID-19 diagnosis: a systematic review and meta-analysis. JAMA Netw Open. 2021;4:
e2137257 . DOIPubMedGoogle Scholar - Australian Government. COVID-19 vaccine roll-out: 01 February 2022 [cited 2023 Jan 30]. https://www.health.gov.au/sites/default/files/documents/2022/02/covid-19-vaccine-rollout-update-1-february-2022.pdf
- Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, et al. Covid-19 vaccine effectiveness against the Omicron (B.1.1.529) variant. N Engl J Med. 2022;386:1532–46. DOIPubMedGoogle Scholar
- Chemaitelly H, Tang P, Hasan MR, AlMukdad S, Yassine HM, Benslimane FM, et al. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N Engl J Med. 2021;385:
e83 . DOIPubMedGoogle Scholar - Kirsebom FCM, Andrews N, Stowe J, Toffa S, Sachdeva R, Gallagher E, et al. COVID-19 vaccine effectiveness against the omicron (BA.2) variant in England. Lancet Infect Dis. 2022;22:931–3. DOIPubMedGoogle Scholar
- Payne RP, Longet S, Austin JA, Skelly DT, Dejnirattisai W, Adele S, et al.; PITCH Consortium. Immunogenicity of standard and extended dosing intervals of BNT162b2 mRNA vaccine. Cell. 2021;184:5699–5714.e11. DOIPubMedGoogle Scholar
- Schmidt T, Klemis V, Schub D, Mihm J, Hielscher F, Marx S, et al. Immunogenicity and reactogenicity of heterologous ChAdOx1 nCoV-19/mRNA vaccination. Nat Med. 2021;27:1530–5. DOIPubMedGoogle Scholar
- Liu X, Shaw RH, Stuart ASV, Greenland M, Aley PK, Andrews NJ, et al.; Com-COV Study Group. Safety and immunogenicity of heterologous versus homologous prime-boost schedules with an adenoviral vectored and mRNA COVID-19 vaccine (Com-COV): a single-blind, randomised, non-inferiority trial. Lancet. 2021;398:856–69. DOIPubMedGoogle Scholar
- Dalton LG, Meder KN, Beard FH, Dey A, Hull BP, Macartney KK, et al. How accurately does the Australian Immunisation Register identify children overdue for vaccine doses? A national cross-sectional study. Commun Dis Intell. 2018;2022:46.
- Government of Western Australia. Proof of COVID-19 vaccination to expand state-wide from Monday 31 January [cited 2023 Jan 30]. https://www.wa.gov.au/government/announcements/proof-of-covid-19-vaccination-expand-state-wide-monday-31-january
Figures
Tables
Cite This ArticleOriginal Publication Date: May 02, 2023
Table of Contents – Volume 29, Number 6—June 2023
| EID Search Options |
|---|
|
|
|
|
|
|




Please use the form below to submit correspondence to the authors or contact them at the following address:
Paul V. Effler, Immunisation Program, Communicable Disease Control Directorate, WA Department of Health, 189 Royal St, East Perth, WA 6004, Australia
Top