Volume 3, Number 4—December 1997
THEME ISSUE
Foodborne
Strategies for Mobilizing Resources for Rapid Response to Emerging Foodborne Microbial Hazards
Foodborne Illness: Implications for the Future
Cite This Article
Citation for Media
Abstract
Many outbreaks of foodborne illness, even those involving newly recognized pathogens, could have been avoided if certain precautions had been taken. This article will draw on existing information to suggest realistic measures that, if implemented, are most likely to avert or diminish the impact of new foodborne disease outbreaks.
I do not see microbiologic infections as totally different from other food hazards, or microorganisms as totally different from other life forms. We are all hosts and prey, parasites and predators. Even though we differ in size, complexity, and weaponry, we employ many similar strategies—the result of a shared planet, and a substantially shared genetic base. That is also why we have much to learn from animal disease surveillance.
Writing on emerging diseases, many argue forcefully for a broad and well-integrated view (1,2); however, aspects absolutely essential to understanding the problem are often omitted. This short article will doubtless make the same error. So, as Shakespeare had Prologue plead at the opening of Henry the Fifth, "Piece out our imperfections in your minds."
Outbreaks occur whenever pathogenic agents in sufficient number or quantity encounter a susceptible population without effective interceptive measures. Then, if we did not expect it, we say "it emerged."
Genetic Variability
The large genetic variability of microorganisms is the principal reason why so often some survive after any unfavorable environmental change. Some strains are hypermutable, which reinforces the potential for survival, and have very short generation times, with bacterial minutes comparable to human years. As Dr. Lederberg notes, microorganisms are opponents with whom we cannot race—on their terms.
Environment
Environmental factors also contribute to emergence. Hot, humid climates favor the growth of fungi and the production of mycotoxins. To borrow an example outside foodborne pathogens, an unusually wet season produced a sharp increase in the deer mice population and the consequent outbreak of hantavirus in the Four Corners area of the United States.
Behavior
Human actions and behavior directly affect food safety. People are vectors for disease, traveling far more often, farther, and more rapidly than ever before (3), and moving far more swiftly than rats, lice, and mosquitoes. Political boundaries frequently and perversely act as leaky sieves, letting diseases through unimpeded, while blocking measures for disease prevention, control, and treatment (1).
Urbanization
Urbanization is a major factor in emergence. Crowding increases human contact and opportunities for transmission. Particularly in developing countries, public health services lag far behind the rush from farm to city. Cities, especially in industrialized nations, are economic and governmental centers and harbor institutions of culture and learning. However, cities are also massive projects in the intensive monoculture of humans. With agriculture, it is entirely possible to carry out monoculture effectively and productively—esthetic considerations aside—if one provides for and tightly controls all essential inputs and conditions, monitors the process closely, and is prepared for prompt and effective intervention if something goes wrong. That hardly describes cities anywhere.
Raw Food Production
The effect of changes in raw food production and harvest practices on opportunities for foodborne outbreaks have been discussed. Centralized processing and wide distribution are the principal characteristics of the "new scenario," as compared to the "old scenario" of local production, home processing, and intrafamily consumption. A classic example is the recent Japanese outbreak of hemorrhagic Escherichia coli.
Denial
A behavior that encourages outbreaks is denying the existence of an epidemic—a practice more common in developing countries concerned about the effect of outbreak publicity on tourist trade and exports (4). One of our own attitudes is indifference to outbreaks perceived as commonplace and distant (5).
Economics
War and economic collapse provide unparalleled opportunities for disease outbreaks (e.g., cholera in central Africa). The infrastructure that provides clean water, community medicine, disease surveillance, and food control, even where it exists, is a fragile fabric, easily torn by economic, social, and physical disruption.
Technology
In spite of their benefits, technologies often bring new or enlarged risks. This is not an argument for returning to a state of nature. The invention of sausage doubtless increased the incidence of botulism; indeed, "botulus" is the Latin word for sausage. Without proper processing, any modern packaging that excludes oxygen can have the same effect.
Risk Factors
Factors such as age, illness, and medical treatment increase the risk for foodborne illness. Such increases also result from behavior that promotes the incidence of other diseases (e.g., AIDS).
Failure to Prevent and Control
The most common human action that adversely affects food safety is the avoidable lack of or failure to use effective prevention and control measures. That failure is why 85% of all outbreaks are traceable, about equally, to mishandling in homes or in food service establishments.
Interacting Factors
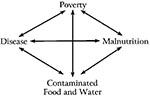
In much of the developing world, an interrelated and mutually reinforcing set of problems keeps foodborne disease at a high level (Figure). Approximately five million children under the age of 5 years living in the tropics die each year of malnutrition and diarrheal disease (6). Palliation is temporary; only economic and technical development can break through this net.
The contributing factors already mentioned would cause us problems, even acting singly. However, they interact, often synergistically. The combination of bacterial genetic variability and the ease and frequency of mutation of strains present a threat because the process enhances selection for new and more dangerous pathogens. Acid rain and recycling through ruminants may have encouraged the increased environmental durability of acid-tolerant E. coli O157:H7. The increasing popularity of marinades in the preparation of foods may have had the same effect.
The globalization of the food trade pulls together several of these contributing factors. One country's contaminated water leads to another country's contaminated raspberries. Refrigeration and controlled atmosphere can preserve pathogens, as well as foods, and spread them all over the world. The Salmonella Enteritidis outbreak from contaminated eggs in ice cream was a typically broad problem.
Technologic change combines many of these contributing factors. The intensive monoculture of plants and animals presents concentrated opportunities. For example, an outbreak of southern corn blight was attributed to the narrow genetic base of a popular hybrid corn. Human-guided plant genetics was defeated by the much more rapid genetic adaptability of microorganisms.
Indiscriminate use of antibiotics and the ability of microorganisms to exchange genetic information has led to increasing resistance. Minimal processing of food, warmly received by natural food lovers, is an open invitation to slightly more durable pathogens to take over the food supply. Centralized processing and mass distribution push us even further in the race Dr. Lederberg reminded us we cannot win. Immunosuppression, due to disease or medication, combined with the failure to take simple sanitary or health precautions make the emergence of pathogens inevitable.
Achieving optimum public health requires many measures, each necessary but not sufficient in itself. The most basic measure is clean water, as recent incidents with strawberries and other fresh produce washed with contaminated water illustrate.
Effective food control structures (e.g., statutory and regulatory frameworks and inspection and enforcement agencies) are essential. A surveillance system has always been required and should be directed to populations at high risk. Newer methods of typing pathogens, faster response times, and enhanced analytical sensitivity are making those systems far more effective than they have been.
Family health programs and education are equally necessary. Food safety still depends heavily on how each of us chooses and uses (or abuses) our food, and each of us is not expert.
We process food for the following main reasons: nutrition, safety, preservation, distribution, and esthetics. Cooking typically increases protein digestibility and destroys antinutrients. Fortification and enrichment add, restore, or increase essential nutrients. Cooking and canning destroy pathogenic organisms; cooking and steeping remove natural toxicants, such as cyanide from cassava. Canning, dehydration, salting, smoking, and preservatives, combined with proper packaging and storage, decrease spoilage. Canning, freezing, refrigeration, and controlled atmosphere storage provide variety and year-round availability. Flavors, colors, pre-sale preparation, and stabilizers that prevent separation or crystallization increase consumer appeal and convenience.
Food Processing Technologies
Food processing technologies reduce our exposure to dietary pathogens in three ways, summarized by Professor E. M. Foster as "the three Ks": keep them out, kill all you can, keep the rest from growing.
One group of technologies removes or destroys microorganisms and naturally occurring toxicants by careful sanitation; heat treatment (e.g., cooking, retorting, pasteurizing, high temperature/short time treatment, ultrahigh temperature treatment, ohmic heating, and other newer techniques); radiation (widely useful and recently applied to all of our current methods); physical separation, (e.g., air separation, gravity tables, visual scanners, and other methods for reducing "natural and unavoidable defects" including gross contamination); dehydration; and new technologies (e.g., hydrostatic pressure, pulsed light).
A second group of technologies keeps contaminants well below dangerous levels. These include raw material quality control; careful sanitation; chemical preservation (i.e., fermentation, bacteriostats, pH control, water activity control, and controlled atmosphere storage); dehydration; and freezing and refrigeration.
The third group of technologies prevents recontamination through sanitation of the general environment and at the point of service, protective packaging, and proper handling to ensure packaging integrity.
Beyond these three groups of technologies are general principles governing the use of all such techniques. All foods require incoming quality control and careful sanitation. For nearly all foods except fresh produce and dried grains, one technology from each group listed above should be used. All technologies used must be applied effectively, or none is effective. These technologies must be used in combination, in a systems approach. Failure to apply properly a preceding technology can cause later technologies to increase microbiologic hazards. If oxygen is later excluded from improperly processed food by packaging (canning, foil, an oil layer), anaerobic pathogens, such as Botulinum, are free to multiply.
Food safety objectives must be established. There is a clear need for priorities and for employing the "principle of commensurate effort" (i.e., applying effort to risks in the order of their probable impact).
There is also the need for a broad view (1,2). The interaction of several factors, not all of which can be seen in advance, makes a team approach essential.
More effort at understanding the evolution of virulence (7) could provide us with insights on the genetic characteristics and the environmental conditions needed to minimize risk. The 1918-19 influenza epidemic can be used as an example; the present search for its genetic makeup suggests the value of prior knowledge. Knowing or estimating the probability of present or future virulence could prepare us for the more effective use of other measures. These include newer, faster, more sensitive methods of detection.
Improved detection would lead to more effective prevention and control measures. The need to establish priorities suggests here, as in cancer research, the value of biomarkers. Biomarkers are genetic or biochemical indicators of impending risk in the potential pathogen, preceding clinical or epidemiologic indications. Such biomarkers might indicate potential virulence, increased environmental durability, or increased resistance to heat, cold, unfavorable pH, preservatives, or antibiotics.
We need to apply available knowledge more effectively. Most outbreaks of foodborne disease are due to mishandling food in ways we already know how to avoid. The points that follow are not new, but as our food supply increases in complexity and geographic reach, these weapons must grow apace.
Clean water, public sanitation, disease surveillance, and food control are more important than ever. The value of effective disease surveillance has been demonstrated. But what we now have and do is not enough. A national response team must be created. Data should be shared more broadly (electronic linkage of laboratory and surveillance results) if we are to cope effectively with a global food supply, multistage processing by different firms at different locations, and national and international distribution. The effective application of these resources requires a Hazard Analysis and Critical Control Points (HACCP) approach (8).
Private health measures must grow in effectiveness and reach. We must make continuing and increasingly effective use of food processing technologies that reduce microbiologic risks. HACCP cannot be generic or static; it must be adapted to each specific product and processing facility and must be updated with continuing feedback on the hazards to be avoided. HACCP, fortified by the public health measures just described and by the results of the research discussed at this conference, will enable the food processing industry to meet the challenges of emerging pathogens.
Even with the steps just described, approximately 85% of all outbreaks occur as a result of food mishandling in food service establishments or homes. We need to extend HACCP principles to the food service sector as well. HACCP probably cannot reach into homes. If we are to communicate better, we need first to find out what consumers already know, what they want to know, and what they need to know. In short, if we are to educate effectively, we must have direct evidence of how well the information process is working.
Finally, we will never succeed in achieving desirable consumer risk-management practices until consumers understand the inevitability of some risks and minimize them. Food risks have been categorized into six groups in decreasing order of size: microbiologic, nutritional, natural toxicant, environmental contaminant, pesticide residues, and food additives (9). The take-home message on food safety for all of us, as consumers, can be summed up in three words: sanitation, variety, moderation. Sanitation deals effectively with microbiologic risks; variety and moderation deal with nutritional risks, minimizing the impact of the four remaining risks to the extent they are even potentially insignificant. Sanitation, variety, and moderation are within our own control as individual consumers. That is doubtless why we have done only a mediocre job of implementing them. Unless all of us can and do pursue these three objectives effectively, we are all at some unnecessarily increased risk.
References
- Farmer P. Social inequalities and emerging infectious diseases. Emerg Infect Dis. 1996;2:259–69. DOIPubMedGoogle Scholar
- Vidaver AK. Emerging and reemerging infectious diseases. American Society for Microbiology News. 1996;62:583.
- Wilson M. Travel and the emergence of infectious diseases. Emerg Infect Dis. 1995;1:39–46. DOIPubMedGoogle Scholar
- Vidaver AK. Emerging and reemerging infectious diseases. American Society for Microbiology News. 1996;62:585.
- Lederberg J, Shope RE, Oaks SC. Emerging infections: microbial threats to health in the United States. Washington (DC): National Academy Press; 1992.
- Snyder JD, Merson MH. The magnitude of the global problem of acute diarrhoeal disease: a review of active surveillance data. Bull World Health Organ. 1996;60:605–13.
- Ewald P. Guarding against the most dangerous emerging pathogens: insights from evolutionary biology. Emerg Infect Dis. 1996;2:245–56. DOIPubMedGoogle Scholar
- International Committee on Microbiological Safety in Foods. HACCP in microbiological safety and quality. In: Microorganisms in Food. Book 4. Oxford: Blackwell Scientific Publications Ltd.; 1988. p. 28-43.
- Wodicka VO. Wodicka rates food additive hazard as low. Food Chemical News. 1971;12:11.
Figure
Cite This ArticleTable of Contents – Volume 3, Number 4—December 1997
| EID Search Options |
|---|
|
|
|
|
|
|