Volume 30, Number 4—April 2024
Research Letter
Successful Treatment of Confirmed Naegleria fowleri Primary Amebic Meningoencephalitis
Cite This Article
Citation for Media
Abstract
Primary amebic meningoencephalitis caused by Naegleria fowleri is a rare but nearly always fatal parasitic infection of the brain. Globally, few survivors have been reported, and the disease has no specific treatment. We report a confirmed case in Pakistan in a 22-year-old man who survived after aggressive therapy.
Naegleria fowleri amebae are thermophilic, free-living, and found in soil and fresh water, such as lakes, rivers, ponds, and untreated swimming pools. The ameba enters the brain through the nose and cribriform plate, causing primary amebic meningoencephalitis. Globally, 381 confirmed cases and only 7 (1.8%) known survivors were reported through 2018 (1). The Centers for Disease Control and Prevention recommends microscopic examination of fresh, unfrozen, nonrefrigerated cerebrospinal fluid (CSF) for presumptive diagnosis (2). If amebae are identified, the diagnosis should be confirmed through PCR. Although no specific treatment for primary amebic meningoencephalitis exists, the Centers for Disease Control and Prevention recommends combination therapy, including intravenous and intrathecal amphotericin B, azithromycin, miltefosine, rifampin, and dexamethasone (2).
N. fowleri ameba poses a substantial problem in Karachi, Pakistan, because of the city’s hot, humid climate in the summer and its coastal location. The first case of N. fowleri infection in Pakistan was reported in 2008, and 146 cases were reported by October 2019 (3). Other than the United States (41.0%), Pakistan has reported the most N. fowleri infections (38.8%) (2).
A 22-year-old man sought care at a secondary-care hospital in Karachi on June 17, 2023, with initial symptoms of fever, drowsiness, and vomiting. He had no history of recreational water sports or swimming. His pulse rate was 105 beats/min, temperature 38.8°C, and blood pressure 121/78 mm Hg. His oxygen saturation was 95% in room air, and he had no respiratory distress. His Glasgow coma score was 11/15; he had neck rigidity, bilateral downgoing planters, and tonic-clonic seizures. Results of laboratory testing were unremarkable except an elevated leukocyte count, 19.3 × 109 cells/mL (reference range 4–10 × 109 cells/mL). We made a provisional diagnosis of acute meningoencephalitis and began empirical therapy with intravenous meropenem (2 g/12 h), intravenous vancomycin (1 g/12 h), intravenous dexamethasone (4 mg/8 h), and sodium valproate (500 mg/12 h).
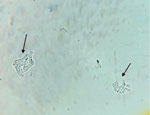
On the same day, we transferred the patient to the intensive care unit of a tertiary-care hospital in Karachi for additional testing and critical care. We sent a CSF sample for microscopic examination, chemical testing, and bacterial culture. The CSF sample was slightly turbid, and test results showed high levels of protein, 950 mg/dL (reference 15–40 mg/dL); glucose, 79.2 mg/dL (reference 50–80 mg/dL); erythrocytes, 52 cells/mm3 (reference 0 cells/mm3); and leukocytes, 162 cells/mm3 (reference 0–5 cells/mm3), with 60% segmented neutrophils. A wet mount of the CSF showed trophozoite forms of an ameba (Figure). We changed the patient’s treatment regimen to oral miltefosine (50 mg/6 h), intravenous amphotericin B (75 mg immediately, then 50 mg/24 h), oral rifampin (400 mg/12 h), intravenous fluconazole (400 mg/12 h), intravenous azithromycin (500 mg/24 h), intravenous sodium valproate (500 mg/8 h), and intravenous 20% mannitol (200 mL/8 h). The patient’s condition began to deteriorate, he had onset of seizures, and his Glasgow coma score dropped to 8/15. We placed him on mechanical ventilation 4 hours after transfer to intensive care.
We sent the CSF sample to the Aga Khan University Reference Laboratory in Karachi for PCR testing. The sample was spun down, and the cell pellet was used for DNA extraction by QIAamp DNA Extraction Kit (QIAGEN, https://www.qiagen.com), according to manufacturer protocol. Real-time PCR was performed using primers targeting the 18S rRNA gene of Naegleria sp., as described previously (4). Parallel PCRs for human RNase P gene, as assay control, and ATCC N. fowleri HB1 (30174D), as positive control, were performed. The PCR testing confirmed the pathogen as N. fowleri ameba.
On day 3, we began intrathecal amphotericin B (15 mg). The intrathecal catheter was accidently removed during nursing care, and we made the decision to discontinue the intrathecal amphotericin B. The clinical course was complicated by ventilator-associated Acinetobacter baumannii pneumonia that was successfully treated with intravenous and inhalational colistin. With combination therapy, the patient’s condition began to improve, and on day 8, he was successfully weaned off mechanical ventilation. He completed a 3-week course of therapy, and on day 28, he was discharged. The patient has since returned to his previous state of health without any neurologic deficit.
A total of 146 cases of N. fowleri amoeba infections were reported in Pakistan during 2008–2019, and only 2 (1.36%) were in patients who had a history of recreational water activity (3). In the patient we describe, the most likely transmission could be ritual ablution with tap water, given that N. fowleri amebae have been isolated in the local domestic water supply (4). Our patient is 1 of only 8 reported laboratory-confirmed N. fowleri survivors worldwide (Table). The survival of our patient could be multifactorial: first, a high index of suspicion led to an early diagnosis, within 24 hours from seeking care to ICU admission; second, we used a combination of antimicrobial drugs, including miltefosine, amphotericin B, rifampin, and azithromycin, administered within 2 hours of diagnosis and ≈48 hours after onset of symptoms.
In conclusion, primary amebic meningoencephalitis caused by N. fowleri amoeba is a rare but fatal disease. A high index of suspicion, early diagnosis, and aggressive combination therapy can help prevent death and long-term illness.
Dr. Burki is a consultant intensive care specialist working in the intensive care unit at PNS Shifa hospital in Karachi, Pakistan.
References
- Gharpure R, Bliton J, Goodman A, Ali IKM, Yoder J, Cope JR. Epidemiology and clinical characteristics of primary amebic meningoencephalitis caused by Naegleria fowleri: a global review. Clin Infect Dis. 2021;73:e19–27. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Naegleria fowleri—primary amebic meningoencephalitis (PAM)—amebic encephalitis. Information for public health and medical professionals [cited 2023 May 3]. https://www.cdc.gov/parasites/naegleria/health_professionals.html
- Ali M, Jamal SB, Farhat SM. Naegleria fowleri in Pakistan. Lancet Infect Dis. 2020;20:27–8. DOIPubMedGoogle Scholar
- Ghanchi NK, Khan E, Khan A, Muhammad W, Malik FR, Zafar A. Naegleria fowleri meningoencephalitis associated with public water supply, Pakistan, 2014. Emerg Infect Dis. 2016;22:1835–7. DOIPubMedGoogle Scholar
- Anderson K, Jamieson A. Primary amoebic meningoencephalitis. Lancet. 1972;2:379. DOIPubMedGoogle Scholar
- Seidel JS, Harmatz P, Visvesvera GS. Successful treatment of PAM. N Engl J Med. 1982;306:346–8. DOIPubMedGoogle Scholar
- Vargas-Zepeda J, Gómez-Alcalá AV, Vásquez-Morales JA, Licea-Amaya L, De Jonckheere JF, Lares-Villa F. Successful treatment of Naegleria fowleri meningoencephalitis by using intravenous amphotericin B, fluconazole and rifampicin. Arch Med Res. 2005;36:83–6. DOIPubMedGoogle Scholar
- Linam WM, Ahmed M, Cope JR, Chu C, Visvesvara GS, da Silva AJ, et al. Successful treatment of an adolescent with Naegleria fowleri primary amebic meningoencephalitis. Pediatrics. 2015;135:e744–8. DOIPubMedGoogle Scholar
- Cope JR, Conrad DA, Cohen N, Cotilla M, DaSilva A, Jackson J, et al. Use of the novel therapeutic agent miltefosine for the treatment of primary amebic meningoencephalitis: report of 1 fatal and 1 surviving case. Clin Infect Dis. 2016;62:774–6. DOIPubMedGoogle Scholar
- Ghanchi NK, Jamil B, Khan E, Ansar Z, Samreen A, Zafar A, et al. Case series of Naegleria fowleri primary ameobic meningoencephalitis from Karachi, Pakistan. Am J Trop Med Hyg. 2017;97:1600–2. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleOriginal Publication Date: March 12, 2024
Table of Contents – Volume 30, Number 4—April 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Dr Luqman Satti, Department of Medical Microbiology, Clinical Pathology Laboratory. National University of Medical Sciences Rawalpindi, Pakistan
Top