Volume 18, Number 4—April 2012
Historical Review
Malaria in Highlands of Ecuador since 1900
Highland Malaria during Construction of Guayaquil to Quito Railway (1890–1945)
Highland Malaria Foci in Ecuador (1900–1950)
Highland Malaria in Northern Valleys (Pichincha and Imbabura) (1940–1950)
Human Colonization of Coastal Foothill Tropical Forests (1950–1970)
History of Malaria Elimination/Control Efforts in Ecuador
Conclusions
Cite This Article
Cite This Article
Citation for Media
Abstract
A recent epidemic of malaria in the highlands of Bolivia and establishment of multiple Anopheles species mosquitoes in the highlands of Ecuador highlights the reemergence of malaria in the Andes Mountains in South America. Because malaria was endemic to many highland valleys at the beginning of the 20th century, this review outlines the 20th century history of malaria in the highlands of Ecuador, and focuses on its incidence (e.g., geographic distribution) and elimination from the northern highland valleys of Pichincha and Imbabura and the role of the Guayaquil to Quito railway in creating highland larval habitat and inadvertently promoting transportation of the vector and parasite. Involvement of control organizations in combating malaria in Ecuador is also outlined in a historical context.
Some authors have speculated that Anopheles mosquitoes may begin transmitting malaria parasites (Plasmodium spp.) at higher altitudes in the South American Andes because of climate change (1,2). In contrast, highland malaria in Africa has more often been attributed to land use alterations, malaria treatment resistance, changes in vector control measures, and human migration into foothill and mountainous regions (3). Before 2004, a short-lived epidemic of P. vivax malaria was recorded in a village in Bolivia at an altitude of 2,300 m that was transmitted by Anopheles pseudopunctipennis Theobald mosquitoes (4). Multiple anopheline malaria vectors have also become established in the highlands of Ecuador (5).
In this review, we summarize documented cases of highland malaria that occurred in Ecuador during the early 20th century. We define the term highland malaria to mean all malaria that occurs in regions with steep topography. Using geographic information systems (ArcGIS version 10; ESRI, Redlands, CA, USA) and tabulated data from historical sources, we reconstruct the geographic extent of malaria incidence during several periods of interest. We also outline malaria control efforts and attempts at malaria elimination for Ecuador during the 20th century and at the beginning of the 21st century.
Although malaria was prevalent on the coast of Ecuador at the beginning of the 20th century, it was considered by public health officials to be a minor problem (6). Until 1908, Guayaquil on the coast of Ecuador was affected by the constant menace of mosquitoes transmitting yellow fever, and flea-borne bubonic plague reoccurred regularly in all areas of the city and surrounding countryside (6–8). Because Guayaquil had an image of being an unhealthy major port city, officials in Ecuador signed an international sanitation convention in 1906 to combat outbreaks of yellow fever, bubonic plague, and cholera (9). Under terms of the convention, officials were to take measures to prevent ongoing transmission of these diseases, including the use of mosquito screens on windows and doors of hospitals (9). During that time, officials also experimented with the use of mosquito larvae–eating fish as a biocontrol method in an attempt to control yellow fever (8).
In 1908, the public health movement became active in Ecuador, and a special sanitary commission was formed in Guayaquil (7,8). At that time, malaria was still considered a minor health problem and many residents allowed mosquitoes to bite them to provide them with long-term immunity to malaria (10). Malaria prevention measures included bed nets, window and door screens, and anopheline larval habitat destruction (8,10). Several medical entomologists became active during this period in Ecuador. These entomologists included the French entomologist Paul Rivet, and the Ecuadorian entomologists F.R. Campos, Luis León, and J. Rodríguez (11).
In 1919, many physicians in Ecuador began to receive training in foreign countries, particularly in the United States through grants from the Rockefeller Foundation, in an attempt to eliminate yellow fever and malaria from Ecuador (6,8,12). With the elimination of yellow fever in 1920, attention inevitably turned to malaria, which still accounted for a large percentage of deaths on the coast of Ecuador (13). By 1940, malaria still remained a priority and was the second leading cause of death in Ecuador after whooping cough (7). At the time, it was recommended that a campaign against malaria should be initiated throughout the entire country (7).
In 1886, construction began on the railway that was to link some of the low-altitude regions of the country near Guayaquil to highland regions and eventually Quito (altitude 2,800 m) (14). The railway was constructed on a route that began in Guayaquil (at sea level), passed through Milagro, and followed the valley bottom up toward Huigra, in Chimborazo (altitude 1,250 m). After Huigra, the railway continued higher toward Alausí, Chimborazo (altitude 2,340 m), after climbing the infamous Devil’s Nose switchbacks (14) (Figure 1).
When construction of the railway reached an elevation of 200 m, workers reported bites from an unidentified bush-dwelling, flying insect and many subsequently died of high fevers (15). At higher altitudes, workers began to report fevers attributed to malaria (14). In 1906, the Guayaquil newspaper Grito del Pueblo reported that railway workers affected by fevers were removed from the construction site and brought to the highland village of Chasqui, Pichincha, for recovery (16). The following quotation from Daniel Barragán, one of the engineers for the railway, provides strong evidence that mosquitoes (Culicidae) were present at worksites: “The mosquitoes were our eternal companions, during all of the night, their melodious and incessant humming many times did not let us find sleep” (translated into English by L.L.P.) (14).
Meitzner described treating many of the railway workers for malaria during 1911 (10). In the winter of that year, the incidence of malaria was so great among workers that construction halted completely (10). Patients were usually brought to higher altitude towns such as Huigra for treatment because there were insufficient medical facilities at lower altitudes (10). Patients with malaria among the railway workers were treated by Meitzner by using a combination of castor oil and quinine and a diet that excluded meat (10). Before operation of the railway, transportation between the coast and highland regions was limited. Therefore, during the early operation of the railway to Quito, the malaria parasite could have been repeatedly introduced by infected passengers and workers to higher altitude regions, including the valleys around the city of Quito (10).
The presence of malaria rather than other similar febrile illnesses in railway workers is further supported by multiple collections of An. pseudopunctipennis larvae (the highland malaria vector) in the Chiripungo Valley, near Alausí, Chimborazo (altitude <2,400 m) (17). As early as 1911, Meitzner made recommendations to railway engineers to construct drainage ditches along the sides of the tracks to prevent establishment of additional larval habitats in the pools that formed there (10). Despite the efforts of Meitzner, An. pseudopunctipennis mosquitoes remained in highland valleys of Chimborazo along the railway at least into the mid 1940s. In 1943, Levi Castillo collected An. pseudopunctipennis larvae along railway tracks up to an altitude of 1,250 m, and in 1944, he collected larvae in pools associated with rivers in the towns of Huigra and Sibambe, Chimborazo (17). These entomologic collections are consistent with the epidemiology of continued malaria transmission; in 1944, a total of 154 cases of malaria among 864 residents were documented in Huigra (18). Aside from habitats associated with the railway line, as shown in Figure 2, partial blockage of the river below the newly built tracks along Devil’s Nose would probably have produced suitable pools for An. pseudopunctipennis larval habitat.
Trains were a likely carrier for continued introduction of anopheline mosquitoes into highland regions from the coast (17,19). At Milagro station, adult mosquitoes were observed to fill train cars bound for higher elevations (19). Levi Castillo found pools of water in ceiling portions of trains, which served as mobile larval habitats for anopheline mosquitoes (17). At higher elevations (>1,100 m), An. pseudopunctipennis mosquitoes were documented as the sole vector, although An. albimanus Wiedemann larvae were collected at lower altitudes along the railway (18). Trains likely served to introduce anopheline mosquitoes to highland regions until the 1960s and 1970s, when the railway fell into disuse (15).
Malaria in highland regions of the northern Andes was not exclusive to Ecuador and was found in Colombia in the Cauca, Manizales, Cali, and Medellín Valleys, and in Peru in the Rimac, Urubamba, and Laurin-Orcocota Valleys (20). Although malaria became more readily studied and possibly more widespread in Ecuador during the 1940s, the vector mosquito An. pseudopunctipennis was likely present for a much longer period in highland regions (21). The malaria parasite is believed to have been introduced to a handful of highland valleys in the 1800s because there are no records of it before that time (22).
In 1905, students at the University of Guayaquil listed the following highland valleys in Ecuador to which malaria was endemic: Imbabura, Chota and Pinampiro valleys in Pichincha; Tumbaco and Guayllabamba Valleys in Tungurahua; the Patate Valley; and the Yunguilla Valley in Azuay (23) (Figure 1). All of these valleys except Patate were regarded as regions to which malaria was endemic into the 1940s (24). In almost every highland valley, Plasmodium vivax was implicated as the only malaria parasite with An. pseudopunctipennis mosquitoes as vectors (11,24).
Highland malaria was widespread in the early 1940s when it appeared to reach its widest distribution (24). In addition to the valleys listed above and highland valleys in Chimborazo associated with the railway, malaria transmission was observed in Imbabura (Mira Valley and Salinas), Pichincha (widespread in all highland valleys), Cañar (all valleys at an elevation <2,500 m), Chimborazo (Pallatanga Valley), Azuay (Yunguilla Valley), and Loja (Catamayo Valley) (11,24) (Figure 1).
In 1938, Hanson and Montalvan documented a new epidemic of P. vivax and P. falciparum malaria in Balzapamba, Bolívar (population 700), in an orange-growing region at an elevation of 650 m (25) (Figure 1). Residents had reportedly never experienced malaria until 1935, although they lived near (≈10 km away) the malaria-endemic coastal plain. In 1935, an earthquake and associated landslides diverted the course of the main river, and an open canal was constructed to provide the town with drinking water (25). Throughout their search, Hanson and Montalvan were able to locate only An. pseudopunctipennis larvae in the open canal and in the algae-covered pools, which formed on the edges of the newly-diverted river (25). This epidemic highlights the scarcity of available larval habitat in steep topography regions and the probable role of river pools and human-made canals as habitat for anopheline larvae in highland regions.
Although An. albimanus mosquitoes have traditionally been considered low-altitude (<300 m) vectors, they were identified as the main malaria vector in an epidemic in the Yunguilla Valley in Azuay (altitude ≈1,500 m) in the late 1940s (17,18). An. pseudopunctipennis mosquitoes were collected from higher-altitude towns in Azuay, such as Santa Isabel, during the 1940s (18). DDT was just beginning to be used at that time in Ecuador and was successfully applied in the 1940s to the Yunguilla Valley (19). During that time, 5% DDT in a solution of kerosene was applied inside homes and to larval habitats (26).
Little research was conducted in southern Ecuador, although there were confirmed malaria cases in the Chota and Pinampiro Valleys in in Imbabura; the Tumbaco and Guayllabamba Valleys in Pichincha; the Patate Valley in Tungurahua; and the Yunguilla Valley in Azuay (18). Montalvan reported his unconfirmed belief that the main vector in Catamayo might be An. punctimacula Dyar mosquitoes, which were otherwise not implicated in highland malaria transmission during the 1940s in Ecuador (18). Similarly, there are few reports of malaria in highland parts of the Amazonian side of the Andes during the early 20th century, likely because the region was sparsely settled. Even in the lower altitude Ecuadorian Amazon communities such as Puyo and Napo (presently Puerto Napo) (altitude 700–900 m), the residents reported no cases of malaria (27) (Figure 1).
Highland malaria in the northern valleys of Ecuador was well documented during its most widespread period (1940–1950) (18,24). Malaria was reported from valleys in Imbabura and Pichincha Provinces, although it never reached the city of Quito (altitude 2,800 m) (24). On the basis of valleys affected and maximum altitudes recorded for anopheline species, the probable extent of highland malaria in the northern valleys during its peak is shown in Figure 3.
Before the widespread occurrence of malaria in the 1940s, Guayllabamba, Pichincha, was considered an area to which malaria was endemic (18,21,22). Gradually, the vector and parasite spread to other valleys, reaching Tingo and Alangasi by 1917 (21) (Figure 1, Figure 3). The spread of malaria may have been in part caused by an exodus of citizens from Guayllabamba during the maximum incidence of the disease (28). When malaria became more widespread in the 1940s, the government in Ecuador brought in the US malariologist Henry Hanson, who identified An. pseudopunctipennis mosquitoes as the only vectors (28). The maximum altitude of the species was estimated to be 2,500 m–2,700 m, although they have since been observed at 3,200 m (11,21,26). An. pseudopunctipennis larvae were collected from clean, sunlit, rocky pools associated with rivers, springs of water, irrigation ditches, and hoof-prints from horses (17,18,20,21). Entomologists also noted a strong larval association with spirogyra algae (18,21,26).
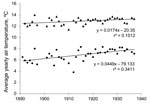
Although the expansion of Anopheles mosquito distribution is often attributed to land use change, highland valleys of northern Ecuador have been cleared and continuously farmed since pre-Colombian times (29). The reported use of river edges as habitats also makes land use change unlikely to be the sole explanation (17,18). Spread of the parasite and vector may also be attributed to meteorologic causes, especially an increase in minimum temperatures, which might otherwise limit parasite or vector development. Increases of 0.5°C in average daily temperature and 1.3°C in minimum nightly temperature were observed in Quito during 1900–1930 (Figure 4). Therefore, meteorologic factors may have caused the increased range of highland malaria before 1940.
A widespread campaign began in 1940 to eliminate malaria from highland valleys of Pichincha and Imbabura (28). Malaria was eliminated in the Los Chillos Valley by the Servicio Antipalúdico del Valle de los Chillos, led by Jaime Rivadeneira, and assisted by Carlos A. Marín and Benjamín Wandemberg (11,17,21,24). A field laboratory was set up in San Pedro de Tingo to lead an initial systematic larval habitat inspection of the entire valley (21). All pools of water used by anopheline larvae were drained by the construction of dikes and sprayed with crude oil mixed with kerosene and occasionally DDT (17,21,28). Smaller pools were filled with earth, and residents were provided with chemical repellent for personal use (17,20). The campaign was deemed a success and malaria did not return in subsequent years (21).
A map of malaria incidence published in 1950 shows the greatest incidence in Ecuador to be in the northern coastal region and An. albimanus, An. pseudopunctipennis, and An. punctimacula mosquitoes to be the most common vectors (31). The foothills of the northern coast were sparsely populated and land was not substantially developed before 1950, because the region was covered in dense tropical forest with limited access (32). However, roads were built linking Quito to the coast in the late 1940s, and settlers moved into the region, forming Santo Domingo (presently Santo Domingo de los Tsáchiles) (altitude ≈500 m) (32). Settlers converted wide swathes of forest to maize, rice, cocoa, and coffee plantations for trade in Quito and in port cities (32). Seasonal workers from the highlands migrated into the region to work during summers (32). The first major epidemic of malaria was reported in 1958 (32). Land conversion likely provided sunlit habitat, which may have been more suitable for some species of Anopheles mosquitoes. Also, the immigration of large groups of highlanders lacking immunity likely contributed to an epidemic in 1958 and to subsequent epidemics.
Although there were several regional public health organizations addressing malaria on the coast of Ecuador, the National Institute of Hygiene and Tropical Medicine Leopoldo Izquieta Pérez was formed in 1940 (33). In 1944, Ecuador had the largest available hospital facilities of any country in Latin America. Physicians were trained by the Pan American Sanitary Bureau with funding from the Rockefeller Foundation, and new public health laboratories were constructed (34,35). In 1948, the Servicio Nacional Antimalárico was formed to campaign against malaria, especially on the coast, and to organize DDT spray operations twice a year (22). In the early 1950s, US organizations led efforts to eradicate malaria from malaria-endemic countries, although insecticide resistance was beginning to appear and slow the eradication progress (36). By 1956, Ecuador was considered to be in an early attack phase of an eradication program (36).
After a recommendation from the Pan American Sanitation Committee, the Sistema Nacional de Eradicación de Malaria (SNEM) was founded on July 21, 1956 (13,22). Its focus was to prevent insect-borne diseases through vector control, mainly through use of chemical insecticides and larval habitat elimination, and public education through school visits, interviews, and community meetings (13). In addition to malaria, SNEM has monitored and controlled Chagas disease, dengue fever, onchocerciasis, yellow fever (in Amazonia), and leishmaniasis in Ecuador (13).
Success of the SNEM in combating malaria has been closely associated with its variable levels of funding. During 1957–1959, dieldrin was sprayed inside houses on a continuous schedule, but was regularly underdosed and therefore not effective (37). During 1961–1965, DDT was applied to houses under the direction of the US Agency for International Development (USAID) and the Pan American Health Organization with greater success (37). Funding for medical entomology research was so poor and unreliable that R. Levi Castillo, who had previously documented many cases of highland malaria, renounced his post at the University of Guayaquil and burned his books in protest (33). By the late 1960s, USAID funding had decreased substantially, resulting in a subsequent epidemic (37). Azuay and Cañar, and to a lesser extent Pichincha and Chimborazo, had a small increase of malaria cases in low-lying valleys (Figure 5). Similarly, in 1969 during another peak year, these highland provinces and most areas of the coast of Ecuador were affected by malaria (Figure 6, panel A).
USAID funding was reinstated in 1973 through a reinvestment with the SNEM (22,37). However, by 1980, the SNEM was considered operational and no longer relied on international funding (37). During an assessment in 1983, the SNEM was deemed to be a capable department but with some financial concerns, such as having an aging fleet of boats and jeeps, and a residual house spray schedule of 3 times a year rather than the recommended 4 times (37).
Through the latter half of the 1980s, some malaria cases were reported in highland provinces of Pichincha, Cotopaxi, Bolívar, and to a lesser extent, Chimborazo and Loja (Figure 5). Tungurahua, Carchi, and Imbabura Provinces reported only occasional malaria cases (Figure 5). During 1 of the peak years (1990), there was widespread malaria along the coast, in Amazonia, and in highland provinces (although perhaps only in lower-altitude regions of these provinces) (Figure 5; Figure 6, panel B). Again in 2000, widespread malaria was observed in the coastal and Amazonian areas of Ecuador (Figure 6, panel C), but only Pichincha and to a lesser extent Cotopaxi and Bolívar observed an increase in cases in the highlands (Figure 5, Figure 6). However, despite occasional cases of malaria, the SNEM reported a steady decrease in malaria in Ecuador during the past 20 years, likely as a response to efforts of various programs that have been more recently implemented in the country (13).
Malaria became more widespread in northern highland regions of Ecuador during 1900–1940 but was subsequently eliminated from these regions through habitat elimination and use of chemical insecticides (21). In Chimborazo during 1900–1950, malaria spread into highland valleys along the railway linking Guayaquil and Quito (10,17,18). Although there have likely been a few highland epidemics since the 1940s, only 1 report in 1991 documented the presence of An. pseudopunctipennis mosquitoes in river-associated habitats of Guayllabamba (28). To effectively monitor establishment of highland malaria vectors, a focus on historically malaria-endemic highland valleys may be needed. Anopheline habitats in areas with steep topography are expected to differ from those in flat, low-altitude regions. Therefore, these differences will necessitate further study of local dynamics of mosquito ecology, meteorologic variables, and transmission cycles.
Dr Pinault just completed her doctorate at Brock University, Canada, studying the ecology of highland Anopheles spp. in the Andes in Ecuador. Her primary research interests include highland malaria, vector ecology, spatial ecology with geographic information systems, and human perspectives of vector-borne diseases.
Dr Hunter is a medical entomologist and professor in the Department of Biological Sciences, Brock University, Canada. Her primary research interests include behavioral and feeding ecology of biting flies, entomologic monitoring for public health, and molecular and chromosomal systematics of Anopheles spp. mosquitoes.
Acknowledgments
We thank Santiago Caizapanta, Julio Rivera, Jady Toscano, Edmundo Caizapanta, Clifford Keil, the staff at Servicio Nacional de Control de Enfermedades Transmitidas por Vectores Artrópodos in Guayaquil, Instituto Nacional de Estadísticas y Censos de Ecuador, G. García Idrovo, and residents of Alausí for assistance.
This study was supported by a Natural Sciences and Engineering Research Council of Canada discovery grant to F.F.H., an International Development Research Centre doctoral research award to L.L.P., and a Natural Sciences and Engineering Research Council of Canada postgraduate scholarship to L.L.P.
References
- Moreno AR. Climate change and human health in Latin America: drivers, effects and policies. Reg Environ Change. 2006;6:157–64. DOIGoogle Scholar
- Reiter P. Climate change and mosquito-borne disease. Environ Health Perspect. 2001;109:141–61.PubMedGoogle Scholar
- Hay SI, Rogers DJ, Randolph SE, Stern DI, Cox J, Shanks GD, Hot topic or hot air? Climate change and malaria resurgence in east African highlands. Trends Parasitol. 2002;18:530–4. DOIPubMedGoogle Scholar
- Rutar T, Baldomar Salgueiro EJ, Maguire JH. Introduced Plasmodium vivax malaria in a Bolivian community at an elevation of 2,300 meters. Am J Trop Med Hyg. 2004;70:15–9.PubMedGoogle Scholar
- Pinault LL, Hunter FF. New highland distribution records of multiple Anopheles species in the Ecuadorian Andes. Malar J. 2011;10:236. DOIPubMedGoogle Scholar
- Pineo RF. Misery and death in the Pearl of the Pacific: Health care in Guayaquil, Ecuador, 1870–1925. Hisp Am Hist Rev. 1990;70:609–37. DOIGoogle Scholar
- Izquieta Pérez L. Public health in Ecuador. Bulletin of the Pan American Sanitary Bureau. 1941;20:1283–5.
- Parks LF, Nuermberger GA. The sanitation of Guayaquil. Hisp Am Hist Rev. 1943;23:197–221. DOIGoogle Scholar
- Sanitary convention [in Spanish]. Grito del Pueblo. 1906 May 13, No. 4227.
- Meitzner M. Malaria, bubonic plague, yellow fever, and ancylostomiasis in Ecuador [in Spanish]. Guayaquil (Ecuador): S.A. Sociedad Filantropica; 1938.
- Astudillo C. Human parasitology [in Spanish]. Quito (Ecuador): Casa de la Cultura Ecuatoriana; 1971.
- Bustamante ME. Public health administration in Latin America. Am J Public Health Nations Health. 1950;40:1067–71. DOIPubMedGoogle Scholar
- Espinoza López N, Triviño Yépez L, Alarcón y Alvarado J, Vélez Nieto L. Technical report: historical and current contribution of the national control of vector-borne disease service (SNEM) for the betterment of the health and the quality of life of Ecuadorians in relation to the illnesses transmitted by arthropod vectors, period 1956–2008 [in Spanish]. Guayaquil (Ecuador): SNEM Technical Commission, Ministry of Public Health, Government of Ecuador; 2009.
- García Idrovo G. The most difficult railway in the world [in Spanish]. Quito (Ecuador): Ministry of Culture, Government of Ecuador; 2008.
- Vásconez VR, Bravo Silva C. Our railway: past, present, future [in Spanish]. Quito (Ecuador); National State Railway Company; 1992.
- From the capital, by telegraph [in Spanish]. Grito del Pueblo. 1906 Mar 17, No. 4170.
- Levi Castillo R. The anophelines of the Republic of Ecuador [in Spanish]. Guayaquil (Ecuador): Artes Graficas Senlieider C.A. Ltda.; 1945.
- Montalvan JA. Malaria in Ecuador [in Spanish]. Guayaquil (Ecuador): Director General of Sanitation, Instituto Nacional de Higiene Leopoldo Izquieta Perez; 1948.
- Levi Castillo R. Studies of the anophelines of the region of Milagro [in Spanish]. Guayaquil (Ecuador): Revista de la Asociación Escuela de Ciencias Quimicas; 1944.
- Levi Castillo R. Studies on the malaria in the Andean valleys of South America [in Spanish]. Revista Médica de Colombia. 1947;15:343–56.
- Levi Castillo R. Anopheles pseudopunctipennis in the Los Chillos valley of Ecuador. J Econ Entomol. 1945;38:385–90.
- Aguilar M. Space and malaria in Ecuador [in Spanish]. In: Aguilar M, Yepez RF, editors. La malaria es más que una picadura. Quito (Ecuador): Instituto Juan Cesar Garcia, Fundación Internacional de Ciencias Sociales y Salud; 1994. p. 1–26.
- (Students of) Huerta B. Malaria [in Spanish]. Guayaquil (Ecuador): Impresora de El Tiempo; 1905.
- Levi Castillo R. The pseudopunctipennis complex in Ecuador (Diptera: Culicidae) [in Spanish]. Guayaquil (Ecuador): Imprenta de la Universidad de Guayaquil; 1944.
- Hanson H, Montalvan JA. Malaria in Balzapamba (epidemiological study) [in Spanish]. Quito (Ecuador): Pan American Sanitation Office; 1938.
- Levi Castillo R. The vectors of malaria of the countries on the coast of the Pacific of South America and their control [in Spanish]. Revista Kuba de Medicina Tropical. 1949;5:101–4.
- Sinclair JH, Wasson T. Explorations in eastern Ecuador. Geogr Rev. 1923;13:190–210. DOIGoogle Scholar
- Gómez de la Torre Serrano JA, Gómez de la Torre Flores P, Cruz ME. Control of malaria at altitude [in Spanish]. In: Cruz ME, de Lourdes Chacon M, editors. New strategies against malaria. Presented at: Conferencia Andina Nuevas Estrategias Contra la Malaria; 1990 May 30–31. Quito (Ecuador): Centro de Documentatción del Sistema de Naciones Unidas Ecuador; 1991. p. 51–7.
- Sarmiento FO. Anthropogenic change in the landscapes of highland Ecuador. Geogr Rev. 2002;92:213–34. DOIGoogle Scholar
- Summary of the meteorological observations made in the observatory and in the diverse stations of the Republic [in Spanish]. Quito (Ecuador): Astronomical and Meteorological Observatory of Quito, Ministry of Public Instruction, Government of Ecuador; 1929–1937; 1937.
- Mackie TT, Hunter GW, Worth CB. Manual of tropical medicine [in Spanish]. 2nd ed. Mexico City: La Prensa Medica Mexicana; 1950.
- Burt AL, Hitchcock CB, James PE, Jones CF, Minkel CW. Santo Domingo de los Colorados – a new pioneer zone in Ecuador. Econ Geogr. 1960;36:221–30. DOIGoogle Scholar
- Barragán AR, Dangles O, Cárdenas RE, Onore G. The history of entomology in Ecuador. Ann Soc Entomol Fr. 2009;45:410–23.
- Perez AR. Cascarilla and its economic importance in Ecuador [in Spanish]. Quito (Ecuador): Publicaciones del Instituto Superior de Pedagogia y Letras; 1944.
- Dunham GC. The cooperative health program of the American Republics. Am J Public Health Nations Health. 1944;34:817–27. DOIPubMedGoogle Scholar
- Russell PF. Malaria in the world today. Am J Public Health Nations Health. 1957;47:414–20. DOIPubMedGoogle Scholar
- Stivers J. Emergency malaria situation in Ecuador. Washington: US Government Report, contract no. 510–0011–0-00–3131–00; 1983.
- INEC (Instituto Nacional de Estatisticas y Censos). Hospital beds and ingressions (national statistical database), 1967–2008 [in Spanish]. Quito (Ecuador): Government of Ecuador; 2008.
- INEC (Instituto Nacional de Estatisticas y Censos). Projection of the population of Ecuador (national statistical database), 1960–2000 [in Spanish]. Quito (Ecuador): Government of Ecuador; 2010.
Figures
Cite This ArticleTable of Contents – Volume 18, Number 4—April 2012
| EID Search Options |
|---|
|
|
|
|
|
|





Please use the form below to submit correspondence to the authors or contact them at the following address:
Lauren L. Pinault, Department of Biological Sciences, Brock University, 500 Glenridge Ave, St. Catharines, Ontario L2T 3K2, Canada
Top