Volume 21, Number 7—July 2015
Dispatch
Outbreak of Ciprofloxacin-Resistant Shigella sonnei Associated with Travel to Vietnam, Republic of Korea
Abstract
We investigated an October 2014 outbreak of illness caused by Shigella sonnei in a daycare center in the Republic of Korea (South Korea). The outbreak strain was resistant to extended-spectrum cephalosporins and fluoroquinolones and was traced to a child who had traveled to Vietnam. Improved hygiene and infection control practices are needed for prevention of shigellosis.
Shigella spp. are etiologic agents of gastrointestinal disease worldwide and are frequently associated with outbreaks because of their low infectious doses and person-to-person transmission (1,2). For the treatment of persons who have severe infections, fluoroquinolones are among the first-line agents for adults; additionally, oral extended-spectrum cephalosporins are used to treat young children. However, the current emergence and spread of drug resistance in Shigella strains could hinder empirical antimicrobial therapy, leading to treatment failure. S. sonnei is the most frequently isolated species among all cases of Shigella infection in industrialized countries (3), and it has become increasingly prevalent across Southeast Asia in recent decades (4). Recently, international travel to areas where the disease is highly endemic has accelerated the global spread of drug-resistant S. sonnei to nonendemic regions. Here, we describe a travel-associated outbreak of illness caused by a S. sonnei strain that was resistant to extended-spectrum cephalosporins and fluoroquinolones.
In the beginning of October 2014, six children who were vomiting and experiencing abdominal cramping and diarrhea were admitted to the local hospital in Gyeongsangnam-do, Republic of Korea (South Korea). All patients attended the same daycare center that provided care and food to children from low-income families. Fecal specimens from 6 patients were submitted to the local public health laboratory and were processed according to a standard bacterial culture method. On October 6, Korea Centers for Disease Control and Prevention was notified that S. sonnei phase II were identified from all fecal samples. An epidemiologic investigation was conducted to determine the extent of the outbreak and to identify the mode of transmission. A confirmed case was identified by passive and active case-finding on the basis of laboratory-identified S. sonnei isolates in the fecal specimens of center attendees and staff members, families of the children, and persons in the community. A probable case was defined as a person with any shigellosis symptoms and an epidemiologic link to infected patients whose cultures were negative. The children’s guardians were interviewed by using a standardized questionnaire that requested information on symptoms, food consumption, recent travel history, and contact persons. This investigation was part of a public health emergency response and was accordingly exempt from institutional review board approval.
The investigation revealed that an 8-year-old boy (the index case-patient in this outbreak) had recently returned after visiting family in Vietnam, where S. sonnei infection is highly endemic. He had experienced sustained diarrheal episodes since his return, and after returning to the daycare center, children in the daycare center began having similar symptoms. Cases of shigellosis were also identified among the grandparents of the index case-patient and a person the family visited in a geographically distant location on September 27. No isolates were obtained from the environmental samples collected, including foods, drinking water, and surface swab specimens of the daycare facility.
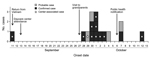
Eleven laboratory confirmed and 4 probable cases were identified during this outbreak. The median age of the patients in the daycare center was 7.8 (range 4–13) years. Overall, the reported symptoms were diarrhea (≥3 loose stools during 24 hours) and abdominal cramping; 4 patients were asymptomatic but their stool samples were culture-positive. Of the 15 persons who became ill (Figure 1), 10 were treated with cefotaxime or ciprofloxacin, after which their stool samples were culture-negative. For 5 patients with continuing positive fecal culture, antibiotic drug treatment was later changed to cabapenems (meropenem or imipenem). According to local infection control guidelines, symptomatic patients were isolated in single-bed rooms until 2 consecutive fecal cultures tested negative for S. sonnei. To prevent the further spread of the disease, public health interventions were encouraged during the outbreak period: enforced handwashing at predetermined times at the daycare facility, strict hygiene measures in affected households, education about shigellosis, and environmental disinfection of the facility.
Laboratory-confirmed strains of S. sonnei were sent to Korea National Institute of Health for further characterization. All 15 isolates had identical or highly similar pulsed-field gel electrophoresis (PFGE) patterns after the XbaI digestion of chromosomal DNA. The main PFGE pattern of this outbreak (SZNX01.183; PFGE pattern number assigned by Korea National Institute of Health) had not been previously reported in domestic cases, and the isolate was genetically indistinguishable from a ciprofloxacin-resistant S. sonnei strain isolated from a traveler returning from Vietnam during 2012 (Figure 2).
On the basis of MICs of antimicrobial agents determined by using a broth microdilution method (5), the outbreak strains were found to be resistant to both extended-spectrum cephalosporins (cefotaxime, MIC >32 μg/mL) and fluoroquinolones (ciprofloxacin, MIC >8 μg/mL). The strains were also resistant to tetracycline and trimethoprim/sulfamethoxazole but were susceptible to chloramphenicol, gentamicin, amikacin, and carbapenem. For azithromycin, an alternative oral agent for shigellosis, MICs were 1–2 μg/mL (Table). Extended-spectrum β-lactamase (ESBL) typing by using PCR and further sequencing (6) showed that all isolates carried the blaCTX-M-15 and blaTEM-1 genes. ESBL plasmid of S. sonnei isolate from the index case-patient were successfully transferred to the recipient E. coli J53 AziR strain. PCR-based inc/rep typing and pMLST analysis of a transconjugant strain (7,8) showed that this ESBL plasmid was of the ST16/IncI1 type, which was previously identified in strain pKHSB1 from Vietnam (9). The genetic environment of the blaCTX-M-15 gene was analyzed by PCR and sequencing with specific primers for the insertion sequences ISEcp1 and orf477 (6). An intact ISEcp1 and truncated orf477 were identified at 48 bp upstream and downstream of the bla gene, which has also been found in CTX-M-15-encoding plasmids from Enterobacteriaceae (6,9,10).
The outbreak strains had 2 mutations in the quinolone resistance-determining region of gyrA (Ser83Leu and Asp87Gly) and 1 mutation in parC (Ser80Ile [Figure 2]), which have been reported to be responsible for ciprofloxacin resistance in S. sonnei (11). However, gyrB and parE mutations and plasmid-mediated quinolone resistance genes were not detected (12).
We describe a shigellosis outbreak affecting children attending a daycare center, their family members, and residents of the surrounding community. To limit the extent of the outbreak, laboratory investigations of outbreak strains and infection-control measures including contact isolation and hand hygiene were immediately implemented, which may have contributed to preventing the further spread of this multidrug-resistant S. sonnei strain.
The outbreak strain was resistant to extended-spectrum cephalosporins and fluoroquinoloness and was introduced by a daycare center attendee who had returned from travel to Vietnam. The blaCTX-M-15 gene in S. sonnei was first described in 2005 (13) and since then has been reported worldwide; we described an outbreak of CTX-M-15–producing S. sonnei in Korea in 2008 (6). The PFGE pattern of the 2008 outbreak strain (SZNX01.176) showed only 82.8% genetic similarity with that of the outbreak strains of the current study but was observed in several traveler-associated cases originating from China. These findings suggest that, despite the lack of direct evidence, various antimicrobial drug–resistant S. sonnei clones have been imported across geographic regions and may eventually spread globally and lead to increased illness and death rates.
In summary, we report a shigellosis outbreak in South Korea caused by a ciprofloxacin-resistant CTX-M-15–producing S. sonnei strain that originated from Vietnam. Because international travel can contribute to the spread of multidrug-resistant pathogens, enhanced surveillance is necessary to control the dissemination of antimicrobial drug resistance. Improved hygiene, infection control plans, and better education for travelers are also required.
Dr Jin Seok Kim is a researcher at Center for Infectious Disease in the Korea National Institute of Health. His primary research interests include antimicrobial drug susceptibility and molecular epidemiology of enteric bacteria.
Acknowledgment
This work was supported by a grant from the Korea Centers for Disease Control and Prevention [4847-311-210].
References
- Kotloff KL, Winickoff JP, Ivanoff B, Clemens JD, Swerdlow DL, Sansonetti PJ, Global burden of Shigella infections: implications for vaccine development and implementation of control strategies. Bull World Health Organ. 1999;77:651–66 .PubMedGoogle Scholar
- Boveé L, Whelan J, Sonder GJ, van Dam AP, van den Hoek A. Risk factors for secondary transmission of Shigella infection within households: implications for current prevention policy. BMC Infect Dis. 2012;12:347. DOIPubMedGoogle Scholar
- Gupta A, Polyak CS, Bishop RD, Sobel J, Mintz ED. Laboratory-confirmed shigellosis in the United States, 1989–2002: epidemiologic trends and patterns. Clin Infect Dis. 2004;38:1372–7. DOIPubMedGoogle Scholar
- Vinh H, Nhu NT, Nga TV, Duy PT, Campbell JI, Hoang NV, A changing picture of shigellosis in southern Vietnam: shifting species dominance, antimicrobial susceptibility and clinical presentation. BMC Infect Dis. 2009;9:204. DOIPubMedGoogle Scholar
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 22nd informational supplement (M100–S22). Wayne (PA): The Institute; 2012.
- Kim JS, Kim J, Jeon SE, Kim SJ, Kim NO, Hong S, Complete nucleotide sequence of the IncI1 plasmid pSH4469 encoding CTX-M-15 extended-spectrum beta-lactamase in a clinical isolate of Shigella sonnei from an outbreak in the Republic of Korea. Int J Antimicrob Agents. 2014;44:533–7. DOIPubMedGoogle Scholar
- Carattoli A, Bertini A, Villa L, Falbo V, Hopkins KL, Threlfall EJ. Identification of plasmids by PCR-based replicon typing. J Microbiol Methods. 2005;63:219–28. DOIPubMedGoogle Scholar
- García-Fernández A, Chiaretto G, Bertini A, Villa L, Fortini D, Ricci A, Multilocus sequence typing of IncI1 plasmids carrying extended-spectrum beta-lactamases in Escherichia coli and Salmonella of human and animal origin. J Antimicrob Chemother. 2008;61:1229–33 . DOIPubMedGoogle Scholar
- Holt KE, Thieu Nga TV, Thanh DP, Vinh H, Kim DW, Vu Tra MP, Tracking the establishment of local endemic populations of an emergent enteric pathogen. Proc Natl Acad Sci U S A. 2013;110:17522–7. DOIPubMedGoogle Scholar
- Woodford N, Carattoli A, Karisik E, Underwood A, Ellington MJ, Livermore DM. Complete nucleotide sequences of plasmids pEK204, pEK499, and pEK516, encoding CTX-M enzymes in three major Escherichia coli lineages from the United Kingdom, all belonging to the international O25:H4–ST131 clone. Antimicrob Agents Chemother. 2009;53:4472–82. DOIPubMedGoogle Scholar
- Folster JP, Pecic G, Bowen A, Rickert R, Carattoli A, Whichard JM. Decreased susceptibility to ciprofloxacin among Shigella isolates in the United States, 2006 to 2009. Antimicrob Agents Chemother. 2011;55:1758–60. DOIPubMedGoogle Scholar
- Ciesielczuk H, Hornsey M, Choi V, Woodford N, Wareham DW. Development and evaluation of a multiplex PCR for eight plasmid-mediated quinolone-resistance determinants. J Med Microbiol. 2013;62:1823–7. DOIPubMedGoogle Scholar
- Lartigue MF, Poirel L, Decousser JW, Nordmann P. Multidrug-resistant Shigella sonnei and Salmonella enterica serotype Typhimurium isolates producing CTX-M β-lactamases as causes of community-acquired infection in France. Clin Infect Dis. 2005;40:1069–70. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 21, Number 7—July 2015
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Junyoung Kim, Division of Enteric Diseases, Center for Infectious Diseases, Korea National Institute of Health, Osong-eup, Heungdeok-gu, Cheongju-si, Chungcheongbuk-do, 363-709, Republic of Korea
Top