Volume 23, Number 9—September 2017
Dispatch
Similarities of Variant Creutzfeldt-Jakob Disease Strain in Mother and Son in Spain to UK Reference Case
Abstract
We investigated transmission characteristics of variant Creutzfeldt-Jakob disease in a mother and son from Spain. Despite differences in patient age and disease manifestations, we found the same strain properties in these patients as in UK vCJD cases. A single strain of agent appears to be responsible for all vCJD cases to date.
In 2008 in Spain, 2 cases of variant Creutzfeldt-Jakob disease (vCJD) in first-degree relatives were identified. After the death of a 41-year-old man (patient 1) from vCJD, his 64-year-old mother (patient 2) began showing symptoms of anxiety and depression and, 2 months later, a gait disorder and progressive dementia. Although the clinical duration was relatively short and the early symptoms uncommon in comparison to vCJD cases in the United Kingdom, the overall clinical phenotype and posterior thalamic hyperintensities as seen in an MRI brain scan led to a diagnosis of suspected vCJD. Neuropathological examination confirmed the diagnosis of vCJD. Both patients were 129MM homozygous, had never received a blood transfusion or tissue graft, and had lived in the same town within the Castilla-León region of Spain (Table 1) (1). The region is a farming area at high risk for bovine spongiform encephalopathy (BSE); 3 of the 5 cases of vCJD reported in Spain came from this region (1). The patients had similar eating habits, which included ingestion of bovine brain. We conducted a study to determine whether these 2 vCJD cases were caused by the BSE agent, whether the agent strain was similar to previously characterized human vCJD cases, and whether the age of the patients would influence the strain characteristics.
We challenged cohorts of mice (RIII, C57BL/6J, and VM) with frozen central nervous system tissue from the 2 patients from Spain and 1 patient originating from the United Kingdom (Table 1) (2). The Lothian NHS Board Research Ethics Committee provided ethical consent for the use of the UK material for research; the vCJD tissue samples from Spain were provided by NEIKER-Tecnalia (Derio, Spain). We conducted inoculation, clinical scoring, and neuropathological and biochemical analysis of the mice as previously described (3–5). Animal studies were conducted according to the regulations of the UK Home Office Animals (Scientific Procedures) Act 1986.
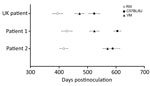
All 3 vCJD brain isolates transmitted successfully, with the appearance of clinical and pathological signs associated with spongiform encephalopathy transmission (Table 2). Inocula from patients 1 and 2 showed the same temporal order of clinical endpoint in each mouse line when compared with inocula from the UK case (Figure 1). We observed a wide range of incubation periods for each mouse line both within and between inocula (Table 2), which is not unusual in primary transmissions.
We generated vacuolation profiles for each mouse line/inocula combination. In RIII and C57BL/6J mice, we observed moderate to mild vacuolation in the medulla and hypothalamus; C57BL/6J mice also exhibited mild vacuolation in the cerebellar peduncle (Figure 2, panels A, B). VM mice showed mild to moderate vacuolation in the medulla, thalamus, and septum, but typically not in the hypothalamus (Figure 2, panel C). Although the distribution of vacuolation was similar between isolates in the different mouse lines, the intensity of vacuolation distribution varied. This difference was most evident in the VM mice, in which the transmission from patient 2 appeared to have a lower intensity of vacuolation than that of patient 1 and the UK patient.
We observed a widespread accumulation of abnormal prion protein (PrP) throughout the brains of inoculated mice, with greatest accumulations apparent in the medulla, hypothalamus, and thalamic areas. We observed variability in the intensity of PrP accumulation between mice both within and between groups. Fine punctate/punctate deposits were the most common form of PrP accumulation in the mice; however, subtle differences were apparent in the hippocampus. In RIII and C57BL/6J, we observed a characteristic PrP deposition in the CA2 region of the hippocampus, whereas VM exhibited PrP deposition in the molecular dentate gyrus with occasional small plaques present in the corpus callosum (Technical Appendix Figure 1).
Biochemical analysis of inocula confirmed the presence of protease-resistant prion protein (PrPres) in each of the 3 isolates. We identified a similar PrPres type in isolates from the Spain patients that resembled that of the UK patient and the vCJD diagnostic standard, with a banding pattern dominated by the diglycosylated fragment of the protein and an unglycosylated fragment of ≈19 kDa (Technical Appendix Figure 2). PrPres was readily detected in the brain of RIII and VM mice challenged with all 3 isolates. We identified a similar glycosylation pattern in both mouse lines; a dominant diglycosylated fragment of ≈30 kDa and an unglycosylated fragment of ≈20k Da. We found no apparent differences between the different mouse line/inocula combinations (Technical Appendix Figure 3).
This transmission study of central nervous system tissue from 2 first-degree relatives with vCJD confirms that the same infectious transmissible spongiform encephalopathy (TSE) agent was responsible for both cases. Comparisons of incubation period, TSE neuropathology, and PrPres biochemistry indicate that this strain is consistent with that of a UK case of vCJD and with historical vCJD transmission data (6). The epidemiologic investigation of the 2 related patients indicated that they had shared a common residence and dietary habits, including cattle brain consumption, for >30 years. This finding suggests a common source of infection linked to the consumption of high-risk material in a known BSE area, and these transmission studies support the hypothesis that consumption of BSE-contaminated food products is a major risk factor for vCJD (7).
A feature of the UK vCJD epidemic was the relatively young age of the patients at onset. During 1995–2014, only 6 of 177 cases of vCJD identified in the United Kingdom were in persons >55 years of age at the onset of symptoms. Clinical phenotypes in these 6 patients were less consistent than those observed in younger patients (8). The evidence suggests that age is not a barrier to either infection or developing the disease; diagnosis of vCJD may become more important as exposed populations become older. Our study demonstrates that older persons harbor the vCJD agent in the central nervous system in a similar manner to younger persons. Small differences in incubation periods and the intensity of TSE vacuolation are apparent, which may be indicative of variation in the titer of the isolates. It is unknown when the 2 patients from Spain were infected, but if they were exposed at the same time, the 23-year difference in age at time of exposure may have influenced pathogenesis and the ability of the agent to replicate. A delay in neuroinvasion or slower rates of replication in the brain could explain why clinical symptoms are more variable in older patients.
Although our study demonstrates that clinical presentation and infective titer may differ between patients, the overall strain characteristics remain similar. Thus, the vCJD strain can be identified using our strain typing panel regardless of these variable factors.
This study highlights the need for awareness of vCJD in older age groups, particularly in patients with clinical manifestations of atypical dementias. These findings add additional supporting evidence to the hypothesis that a single strain of TSE agent is responsible for vCJD cases, regardless of geographic origin or age at infection, and indirectly support the hypothesis of a dietary origin for primary cases of vCJD.
Dr. Diack is a Career Track Fellow at The Roslin Institute, University of Edinburgh. Her research interests focus on prion diseases, in particular strain characterization and modeling of human diseases.
Acknowledgments
We thank the Biomedical Research Facility of The Roslin Institute for animal care and the Pathology staff of R(D)SVS for sectioning the mouse brains. We thank Emma Hunt for technical support.
Tissue samples were acquired through the Edinburgh Brain Bank, which is supported by the Medical Research Council (MR/L016400/1).
This report is independent research commissioned and funded by the Department of Health Policy Research Programme (Strain typing of vCJD). The views expressed in this publication are those of the author(s) and not necessarily those of the Department of Health.
References
- Riverol M, Palma J-A, Alañá M, Guerrero-Márquez C, Luquin MR, Rábano A. Variant Creutzfeldt-Jakob disease occurring in mother and son. J Neurol Neurosurg Psychiatry. 2012;83:235–6 . DOIPubMedGoogle Scholar
- Heath CA. Clinical aspect of variant CJD in the UK 1995–2005. University of Aberdeen; 2008.
- Diack AB, Ritchie D, Bishop M, Pinion V, Brandel JP, Haik S, et al. Constant transmission properties of variant Creutzfeldt-Jakob disease in 5 countries. Emerg Infect Dis. 2012;18:1574–9. DOIPubMedGoogle Scholar
- Dickinson AG, Meikle VMH, Fraser H. Identification of a gene which controls the incubation period of some strains of scrapie agent in mice. J Comp Pathol. 1968;78:293–9. DOIPubMedGoogle Scholar
- Fraser H, Dickinson AG. The sequential development of the brain lesion of scrapie in three strains of mice. J Comp Pathol. 1968;78:301–11. DOIPubMedGoogle Scholar
- Ritchie DL, Boyle A, McConnell I, Head MW, Ironside JW, Bruce ME. Transmissions of variant Creutzfeldt-Jakob disease from brain and lymphoreticular tissue show uniform and conserved bovine spongiform encephalopathy-related phenotypic properties on primary and secondary passage in wild-type mice. J Gen Virol. 2009;90:3075–82. DOIPubMedGoogle Scholar
- Ward HJ, Everington D, Cousens SN, Smith-Bathgate B, Leitch M, Cooper S, et al. Risk factors for variant Creutzfeldt-Jakob disease: a case-control study. Ann Neurol. 2006;59:111–20. DOIPubMedGoogle Scholar
- el Tawil S, Mackay G, Davidson L, Summers D, Knight R, Will R. Variant Creutzfeldt-Jakob disease in older patients. J Neurol Neurosurg Psychiatry. 2015;86:1279–80. DOIPubMedGoogle Scholar
Figures
Tables
Cite This Article1These senior authors contributed equally to this article.
Table of Contents – Volume 23, Number 9—September 2017
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Abigail B. Diack, The Roslin Institute, Easter Bush, Scotland, UK
Top