Volume 24, Number 5—May 2018
Dispatch
External Quality Assessment for Zika Virus Molecular Diagnostic Testing, Brazil
Abstract
We conducted an external quality assessment of Zika virus molecular diagnostic tests in Brazil using a new Zika virus standard. Of 15 laboratories, 73% showed limited sensitivity and specificity. Viral load estimates varied significantly. Continuous quality assurance is required for adequate estimates of Zika virus–associated disease and determination of patient care.
The catastrophic Zika virus outbreak in the Americas has affected millions of persons. Brazil was the most affected country and reported ≈95% of all cases of suspected Zika virus–associated congenital disease (1). Limited sensitivity and specificity of tests hampers serologic detection of Zika virus–specific antibodies in tropical regions (2). Thus, real-time reverse transcription PCR (RT-PCR) has been key for diagnosing acute Zika virus infection and for use in epidemiologic studies (3–5). However, Zika virus molecular diagnostic testing is challenged by short-term viremia and low viral loads (3).
A recent external quality assessment (EQA) in Europe revealed that 60% of laboratories need to improve molecular Zika virus detection (6). Laboratories in affluent countries conduct Zika virus diagnostic testing predominantly in travelers returning from tropical regions. In resource-limited settings to which multiple co-circulating arboviruses are endemic, the diagnostic demands differ entirely. To evaluate the diagnostic landscape in the region most affected by Zika virus, we performed an EQA of molecular Zika virus diagnostic testing in Brazil during 2017.
Fifteen laboratories from 7 Brazilian states participated in this study; these laboratories are spread across ≈2,500 km longitude, including the areas most affected during Brazil’s Zika virus outbreak (1). Participants were university laboratories, hospital laboratories, federal research institutes supporting public health services, and a diagnostic testing company. We provided EQA panels to all laboratories. Each panel comprised 12 lyophilized samples containing inactivated full virus spiked into human plasma tested negative for arboviruses beforehand. The panel consisted of 4 Zika virus–positive specimens of 103–106 RNA copies/mL to assess sensitivity and determine viral load. Zika virus–negative specimens to assess specificity comprised dengue virus serotypes 2 and 4, Japanese encephalitis virus, St. Louis encephalitis virus, West Nile virus, yellow fever virus, and chikungunya virus at ≈105 50% tissue culture infective dose/mL each and a negative plasma specimen (Table 1). Moreover, each panel included the international World Health Organization (WHO) Zika virus standard for quantification (7). However, the WHO standard has limited availability. Importation of the WHO standard may be restricted by countries that perceive heat-inactivated materials that derive from live virus as potentially infectious. Therefore, we designed and acquired a Zika virus armored RNA (Asuragen, Austin, TX, USA). The Zika virus armored RNA is a synthetic RNA covering the target sites of 9 Zika virus–specific real-time RT-PCRs as described previously (3), encapsulated into bacteriophage proteins. This highly stable, noninfectious, pseudoviral particle can be used as a universal control for the covered assays, shipped without biosafety concerns, and used as a control for both nucleic acid preparation and RT-PCR.
We asked all laboratories to conduct molecular Zika virus diagnostics as routinely done with clinical samples and to quantify Zika virus–positive specimens using both standards. All but 1 laboratory used the same real-time RT-PCR protocol developed by Lanciotti et al. (2), highlighting the wide dissemination of this assay in Brazil and suggesting comparability of test results within this study (Table 1). We found no significant difference between samples containing comparable quantities of the Asian and the African Zika virus lineage, suggesting suitability of the protocols for both lineages (p = 0.313 by Fisher exact test).
EQA results varied among laboratories. Of 15 laboratories, 4 (27%) reported correct results for all samples. Five (33%) reported 1 or 2 false-negative results from samples with low Zika virus concentrations (Table 1; Figure 1, panel A). EQA participants correctly tested only the 2 samples containing the highest Zika virus concentrations of 8.1 × 105 and 7.0 × 103 copies/mL (exact test of goodness-of-fit p = 1.00 and p = 0.14, respectively). This finding suggests a potential lack of sensitivity that may be problematic given that viral loads of 103–104 copies/mL are commonly observed in Zika virus–infected patients (3).
Six (40%) laboratories reported >3 false results, including at least 2 false-positive detections of Zika virus–negative specimens. No heterologous flavivirus was particularly affected by false-positive detection, suggesting that false-positive results did not result from unspecific binding of assay oligonucleotides (Table 1). Instead, false-positive results hint at the possibility of laboratory contamination potentially resulting from virus isolation attempts or PCR amplicons generated during prior Zika virus experimentation.
EQA performance varied according to the way viral RNA was prepared. The 8 laboratories conducting Zika virus detection using automated platforms performed generally superior (n = 8; Youden index, 0.661) compared with the 7 laboratories conducting manual RNA extraction (Youden index, 0.446) (Table 2). This finding might indicate an increased risk for contamination during manual RNA preparation. However, automated RNA preparation also might represent a proxy for more affluent settings of those laboratories.
As previously reported (3), RNA extraction critically influences the clinical lower limit of detection (LOD). Although all participants used highly sensitive real-time RT-PCRs, clinical LODs varied considerably because of different RNA extraction protocols (Figure 1, panel B). Lack of detection of low-concentration EQA samples is thus not surprising because even a small decrease in sensitivity readily causes clinical LODs above the concentration of the lowest EQA panel specimen (Figure 1, panel C). This finding highlights that optimized RNA extraction protocols are crucial for sensitive Zika virus diagnostics.
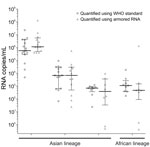
Quantification of Zika virus loads did not differ significantly between use of the armored RNA and the WHO Zika virus standard, with only 0.76 log10 median deviation between results (p = 0.429 by Wilcoxon signed rank test). This observation suggests usability of the armored RNA for Zika virus quantification in tropical regions. Irrespective of the standard, viral load determinations among laboratories were comparable with 0.12–0.88 log10 median deviations of viral load estimates among laboratories for individual Zika virus specimens. However, we also observed drastic deviations of up to 6 orders of magnitude (Figure 2), suggesting that caution must be taken upon comparing viral load determinations as markers for severe Zika virus disease (8,9) among different laboratories.
Some laboratories in Brazil showed suboptimal sensitivity and specificity of Zika virus diagnostic testing. However, these laboratories performed comparably to those in Europe (6). Neither sensitivity nor specificity differed significantly between laboratories in Brazil compared with those in Europe (p = 0.767 and p = 0.324, respectively, by Fisher exact test). Similarly, the proportion of perfectly performing laboratories in this EQA (27%) was comparable with previous EQAs of flavivirus molecular diagnostics, including yellow fever virus (18%), dengue virus (24%), and West Nile virus (27%) (10–12). Flavivirus molecular diagnostics are thus generally challenging and benefit greatly from controls, such as those provided in this EQA. This study underscores the need to combine RT-PCR and serologic testing in Zika virus diagnostic testing, despite their inherent limitations (3).
Independently of the challenges of Zika virus molecular detection, because of taxation and distributor margins, RT-PCR reagents in Latin America are usually 100%–200% more expensive than in affluent countries (13). Limited resources and relatively higher costs potentially force laboratories in Brazil to seek inferior, more affordable solutions. Enhanced access of laboratories in tropical regions to state-of-the-art reagents is thus an unresolved key component of outbreak response. Further EQAs in Brazil should involve state laboratories that carry a large proportion of Zika virus testing within the public health care system. Unfortunately, the state laboratories we contacted for this EQA could not participate because of limited resources.
Finally, lack of sensitivity directly affects estimates of the absolute risk for Zika virus–induced congenital disease upon maternal infection during pregnancy (14). False-positive results potentially have dramatic consequences for patients, as illustrated by a >90% increase in illegal abortion requests in Latin America during the 2016 Zika virus epidemic (15). Our results emphasize the need for continuous quality assessments of Zika virus diagnostic testing globally.
Mr. Fischer is a PhD student at the Institute of Virology at Charité-Universitätsmedizin, Berlin, Germany, and the German Centre for Infection Research, Germany. His main research interests are diagnostics of emerging arboviruses.
Acknowledgments
We thank Michaele Josten, Monika Eschbach-Bludau, and Stefan Holtin for technical support.
The Zika virus armored RNA standard is available for noncommercial use for quality assurance at the EVAg portal (https://www.european-virus-archive.com/)
This work was supported by the German Centre for Infection Research through a fast-track program for Zika virus outbreak response to J.F.D. and is partially supported by the European Union’s Horizon 2020 research and innovation program (ZIKAlliance, grant agreement no. 734548 to X.d.L. and EVAg, grant agreement no. 653316 to C.D.).
References
- de Oliveira WK, de França GVA, Carmo EH, Duncan BB, de Souza Kuchenbecker R, Schmidt MI. Infection-related microcephaly after the 2015 and 2016 Zika virus outbreaks in Brazil: a surveillance-based analysis. Lancet. 2017;390:861–70. DOIPubMedGoogle Scholar
- Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–9. DOIPubMedGoogle Scholar
- Corman VM, Rasche A, Baronti C, Aldabbagh S, Cadar D, Reusken CB, et al. Assay optimization for molecular detection of Zika virus. Bull World Health Organ. 2016;94:880–92. DOIPubMedGoogle Scholar
- Brasil P, Pereira JP Jr, Moreira ME, Ribeiro Nogueira RM, Damasceno L, Wakimoto M, et al. Zika virus infection in pregnant women in Rio de Janeiro. N Engl J Med. 2016;375:2321–34. DOIPubMedGoogle Scholar
- de Araújo TVB, Rodrigues LC, de Alencar Ximenes RA, de Barros Miranda-Filho D, Montarroyos UR, de Melo APL, et al.; investigators from the Microcephaly Epidemic Research Group; Brazilian Ministry of Health; Pan American Health Organization; Instituto de Medicina Integral Professor Fernando Figueira; State Health Department of Pernambuco. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: preliminary report of a case-control study. Lancet Infect Dis. 2016;16:1356–63. DOIPubMedGoogle Scholar
- Charrel R, Mögling R, Pas S, Papa A, Baronti C, Koopmans M, et al. Variable sensitivity in molecular detection of Zika virus in European expert laboratories: external quality assessment, November 2016. J Clin Microbiol. 2017;55:3219–26. DOIPubMedGoogle Scholar
- Baylis SA, Hanschmann KO, Schnierle BS, Trösemeier JH, Blümel J; Zika Virus Collaborative Study Group. Harmonization of nucleic acid testing for Zika virus: development of the 1stWorld Health Organization International Standard. Transfusion. 2017;57(3pt2):748–61. DOIPubMedGoogle Scholar
- Halai UA, Nielsen-Saines K, Moreira ML, de Sequeira PC, Junior JPP, de Araujo Zin A, et al. Maternal Zika virus disease severity, virus load, prior dengue antibodies, and their relationship to birth outcomes. Clin Infect Dis. 2017;65:877–83. DOIPubMedGoogle Scholar
- Terzian ACB, Schanoski AS, Mota MTO, da Silva RA, Estofolete CF, Colombo TE, et al. Viral load and cytokine response profile does not support antibody-dependent enhancement in dengue-primed Zika virus–infected patients. Clin Infect Dis. 2017;65:1260–5. DOIPubMedGoogle Scholar
- Domingo C, Escadafal C, Rumer L, Méndez JA, García P, Sall AA, et al. First international external quality assessment study on molecular and serological methods for yellow fever diagnosis. PLoS One. 2012;7:e36291. DOIPubMedGoogle Scholar
- Domingo C, Niedrig M, Teichmann A, Kaiser M, Rumer L, Jarman RG, et al. 2nd International external quality control assessment for the molecular diagnosis of dengue infections. PLoS Negl Trop Dis. 2010;4:e833. DOIPubMedGoogle Scholar
- Niedrig M, Linke S, Zeller H, Drosten C. First international proficiency study on West Nile virus molecular detection. Clin Chem. 2006;52:1851–4. DOIPubMedGoogle Scholar
- Drexler JF, Kupfer B, Petersen N, Grotto RM, Rodrigues SM, Grywna K, et al. A novel diagnostic target in the hepatitis C virus genome. PLoS Med. 2009;6:e31. DOIPubMedGoogle Scholar
- Moreira-Soto A, Sarno M, Pedroso C, Netto EM, Rockstroh A, Luz E, et al. Evidence for congenital Zika virus infection from neutralizing antibody titers in maternal sera, north-eastern Brazil. J Infect Dis. 2017;216:1501–4. DOIPubMedGoogle Scholar
- Aiken AR, Scott JG, Gomperts R, Trussell J, Worrell M, Aiken CE. Requests for abortion in Latin America related to concern about Zika virus exposure. N Engl J Med. 2016;375:396–8. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 24, Number 5—May 2018
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Jan Felix Drexler, Helmut-Ruska-Haus, Institute of Virology, Campus Charité Mitte, Charitéplatz 1, 10098 Berlin, Germany
Top