Volume 27, Number 12—December 2021
Dispatch
SARS-CoV-2–Specific Antibodies in Domestic Cats during First COVID-19 Wave, Europe
Cite This Article
Citation for Media
Abstract
We conducted a severe acute respiratory syndrome coronavirus 2 antibody seroprevalence study among >2,000 domestic cats from 4 countries during the first coronavirus disease wave in Europe. We found 4.4% seroprevalence using a virus neutralization test and 4.3% using a receptor-binding domain ELISA, demonstrating probable human-to-cat transmission.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of the ongoing coronavirus disease (COVID-19) pandemic, causes high rates of illness and death among humans. SARS-CoV-2 is a newly recognized member of the genus Betacoronavirus, family Coronaviridae, that infects humans. An early serosurvey among domestic cats in Wuhan, China, during January–March 2020 reported 14.7% seropositivity (1). Experimental infections demonstrated susceptibility to SARS-CoV-2 infection in cats and other carnivore species, such as ferrets (Mustela putorius furo), minks (Neovison vison), and to a lesser extent domestic dogs (2,3), and confirmed anecdotal observations of naturally occurring human-to-animal transmissions (4,5). Respiratory and gastrointestinal signs were observed in SARS-CoV-2–infected cats (6–8). We conducted a seroprevalence study for SARS-CoV-2–specific antibodies among domestic cats in Europe during and after the first COVID-19 pandemic wave, using a plaque-reduction virus neutralization test (VNT) and a SARS-CoV-2 receptor-binding domain–specific ELISA (RBD-ELISA).
We analyzed serum samples collected from 2,160 domestic cats during April–June 2020. Samples had been sent to a veterinary diagnostic laboratory (LABOklin; Kissingen, Germany) for diagnostic purposes unrelated to suspicion of SARS-CoV-2 infection (9). Samples were from 1,136 cats in Germany, 331 in the United Kingdom, 333 in Italy, and 360 in Spain. Among 1,799 samples with demographic data, cats ranged from 0.1–23 years of age (median and mean age 11 years). We estimated a minimum of 300 total samples per location to enable a realistic estimation for each location. To confirm specificity of the assays to detect SARS-CoV-2–specific antibodies, we included 25 prepandemic cat serum samples and 25 serum samples from cats that tested positive for feline coronavirus/feline infectious peritonitis (FCoV/FIP) by NovaTec VetLine (Novatec Immundiagnostica GmbH, https://www.novatec-id.com), a commercial antibody test, in the screening.
We tested all serum samples by VNT, as previously described (10). We considered serum samples positive when titers were >20, expressed as the reciprocal of the dilution that gave >80% reduction of stained cells in the plaque reduction neutralization test (PRNT80) (Appendix).
We also tested serum samples with an indirect ELISA we developed and validated inhouse. We used an ELISA previously used for detecting SARS-CoV-2 RBD antibodies in human serum (11) and replaced the anti-human IgG conjugate with an anti-cat IgG conjugate (Appendix).
We evaluated performance characteristics of the cat ELISA-RBD by using Pearson correlation of the results obtained by ELISA-RBD and Gaussian distribution analyses for the VNT. We also calculated diagnostic sensitivity and specificity of the ELISA-RBD compared with VNT. We conducted data analyses using R (R Foundation for Statistical Computing, https://www.r-project.org) and Prism version 9 (GraphPad Software Inc., https://www.graphpad.com). We calculated SARS-CoV-2 seroprevalence in cats separately for each country.
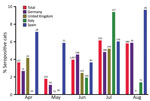
We found overall SARS-CoV-2 seroprevalence among cats was 4.2% in Germany, 3.3% in the United Kingdom, 4.2% in Italy, and 6.4% in Spain (Table 1; Figure). Among all 2,160 cat serum samples tested, 96 (4.4%, 95% CI 3.6%–5.4%) were positive by VNT and 92 (4.3%, 95% CI 3.4%–5.2%) by RBD-ELISA. The RBD-ELISA showed a diagnostic sensitivity of 90.6% (95% CI 90.0%–91.2%) and specificity of 99.8% (95% CI 99.8%–99.8%) compared with VNT (Table 2). Furthermore, correlation (r = 0.9, 95% CI 0.9–0.9) and Gaussian distribution analyses (r2>0.7) revealed high agreement between VNT and RBD-ELISA sensitivities. All 25 prepandemic serum samples and 25 FCoV/FIP-positive samples tested SARS-CoV-2–negative in both the VNT and RBD-ELISA (data not shown), confirming the specificity of the assay for measuring SARS-CoV-2–specific antibodies.
Our study of domestic cat serum from 4 selected countries showed that during the first COVID-19 wave in Europe, >4% of domestic cats had been infected with SARS-CoV-2, probably through their contacts with infected humans. Because serum samples were sent to the veterinary diagnostic laboratory for conditions unrelated to a suspected SARS-CoV-2 infection, our data might not fully represent the overall seropositivity of the domestic cat population in Europe.
We used a VNT and an RBD-ELISA based on the original SARS-CoV-2 wild-type isolate (Wuhan-Hu-1, GenBank accession no. MN908947.3). The RBD-ELISA proved to have a high sensitivity and specificity compared with the VNT (Table 2), but 5 low-titer (titer = 20) VNT-positive samples remained undetected by the RBD-ELISA. These samples might have remained undetected because of the high specificity of RBD-ELISA, which detects antibodies toward the single spike protein ectodomain. Unlike RBD-ELISA, VNT might identify a broader range of virus neutralizing antibodies, including those directed against other domains of the spike protein. Of note, the only correlation of virus protection we have to date is virus neutralization, which apparently correlates well with RBD-ELISA positivity. For serologic screening and for individual diagnostic testing of domestic cats, the RBD-ELISA could replace the VNT, thus avoiding the use of live SARS-CoV-2 under Biosafety Level 3 laboratory conditions. We further confirmed specificities of the VNT and RBD-ELISA by showing that prepandemic and FCoV/FIP-positive cat serum samples were negative in both assays. This finding excluded the detection of cross-reactive antibodies against feline alphacoronaviruses (4) and alphacoronaviruses of other animal species that might infect cats (4,12). Our data contrast a heavily affected area in China at the onset of the pandemic from which seropositivity levels of domestic cats ranged <15% (1), although those results were from relatively fewer tested cats and used a different assay.
During the first COVID-19 pandemic wave, reported seroprevalence levels in domestic cats ranged from 0.4% in the Netherlands (4) to 23% among cats in COVID-19–positive households in France (13). Similar seroprevalence levels in cats and humans in the same areas found by us and others suggest that in the absence of another known source (4,13; C. Schulz, unpublished data) (Appendix Table), SARS-CoV-2 infections in cats are most likely due to human-to-cat contact transmission.
Most natural SARS-CoV-2 infections of cats appear to run a mild or subclinical course, with respiratory or gastrointestinal clinical signs reported in confirmed natural infections (6–8). Evidence from experimental studies suggests that cats are susceptible to SARS-CoV-2 infection and can maintain the virus within a cat population and spill the infection backward or forward to other species (2,3,14). However, no evidence of cat-to-human transmission, nor of cat-specific mutations or variants of SARS-CoV-2, has been detected thus far (8,12,15). This finding contrasts reports on minks kept in farms, where mink-to-human spillback infections and mink-specific mutations have been reported (5). Although no evidence currently suggests that domestic cats play a role in the epidemiology of human SARS-CoV-2 infection, clinicians and veterinary practitioners should recommend that SARS-CoV-2–infected persons avoid close contact with their domestic cats and practice the same nonpharmaceutical prevention measures toward cats as they do to prevent human-to-human infection.
Dr. Schulz is a postdoctoral researcher at University of Veterinary Medicine Hannover, Hannover, Germany. Her research interests include the pathogenesis and epidemiology of emerging and vectorborne diseases. Dr. Martina is a senior researcher at Artemis One Health Research Foundation, Delft, the Netherlands. His research interests include the pathogenesis of and intervention strategies against emerging virus infections.
Acknowledgment
This study was supported in part by the Ministry of Science and Culture of Lower Saxony in Germany (grant no. 14-76103-184 CORONA-15/20). This publication was supported by the DFG and the University of Veterinary Medicine Hannover Foundation within the funding program Open Access Publishing.
References
- Zhang Q, Zhang H, Gao J, Huang K, Yang Y, Hui X, et al. A serological survey of SARS-CoV-2 in cat in Wuhan. Emerg Microbes Infect. 2020;9:2013–9. DOIPubMedGoogle Scholar
- Bosco-Lauth AM, Hartwig AE, Porter SM, Gordy PW, Nehring M, Byas AD, et al. Experimental infection of domestic dogs and cats with SARS-CoV-2: Pathogenesis, transmission, and response to reexposure in cats. Proc Natl Acad Sci U S A. 2020;117:26382–8. DOIPubMedGoogle Scholar
- Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016–20. DOIPubMedGoogle Scholar
- Zhao S, Schuurman N, Li W, Wang C, Smit LAM, Broens EM, et al. Serologic screening of severe acute respiratory syndrome coronavirus 2 infection in cats and dogs during first coronavirus disease wave, the Netherlands. Emerg Infect Dis. 2021;27:1362–70. DOIPubMedGoogle Scholar
- European Centre for Disease Prevention and Control. Detection of new SARS-CoV-2 variants related to mink–12 November 2020 [cited 2021 May 28]. https://www.ecdc.europa.eu/sites/default/files/documents/RRA-SARS-CoV-2-in-mink-12-nov-2020.pdf
- Sailleau C, Dumarest M, Vanhomwegen J, Delaplace M, Caro V, Kwasiborski A, et al. First detection and genome sequencing of SARS-CoV-2 in an infected cat in France. Transbound Emerg Dis. 2020;67:2324–8. DOIPubMedGoogle Scholar
- Garigliany M, Van Laere AS, Clercx C, Giet D, Escriou N, Huon C, et al. SARS-CoV-2 natural transmission from human to cat, Belgium, March 2020. Emerg Infect Dis. 2020;26:3069–71. DOIPubMedGoogle Scholar
- Hosie MJ, Epifano I, Herder V, Orton RJ, Stevenson A, Johnson N, et al.; COVID-19 Genomics UK (COG-UK) consortium. Detection of SARS-CoV-2 in respiratory samples from cats in the UK associated with human-to-cat transmission. Vet Rec. 2021;188:
e247 . DOIPubMedGoogle Scholar - Nørgaard SK, Vestergaard LS, Nielsen J, Richter L, Schmid D, Bustos N, et al. Real-time monitoring shows substantial excess all-cause mortality during second wave of COVID-19 in Europe, October to December 2020. Euro Surveill. 2021;26:
2002023 . DOIPubMedGoogle Scholar - Wang C, Li W, Drabek D, Okba NMA, van Haperen R, Osterhaus ADME, et al. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat Commun. 2020;11:2251. DOIPubMedGoogle Scholar
- Okba NMA, Müller MA, Li W, Wang C, GeurtsvanKessel CH, Corman VM, et al. Severe acute respiratory syndrome coronavirus 2–specific antibody responses in coronavirus disease patients. Emerg Infect Dis. 2020;26:1478–88. DOIPubMedGoogle Scholar
- Hosie MJ, Hofmann-Lehmann R, Hartmann K, Egberink H, Truyen U, Addie DD, et al. Anthropogenic infection of cats during the 2020 COVID-19 pandemic. Viruses. 2021;13:185. DOIPubMedGoogle Scholar
- Fritz M, Rosolen B, Krafft E, Becquart P, Elguero E, Vratskikh O, et al. High prevalence of SARS-CoV-2 antibodies in pets from COVID-19+ households. One Health. 2021;11:
100192 . DOIPubMedGoogle Scholar - Halfmann PJ, Hatta M, Chiba S, Maemura T, Fan S, Takeda M, et al. Transmission of SARS-CoV-2 in domestic cats. N Engl J Med. 2020;383:592–4. DOIPubMedGoogle Scholar
- Barrs VR, Peiris M, Tam KWS, Law PYT, Brackman CJ, To EMW, et al. SARS-CoV-2 in quarantined domestic cats from COVID-19 households or close contacts, Hong Kong, China. Emerg Infect Dis. 2020;26:3071–4. DOIPubMedGoogle Scholar
Figure
Tables
Cite This ArticleOriginal Publication Date: October 25, 2021
1These authors contributed equally to this article.
Table of Contents – Volume 27, Number 12—December 2021
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Albert Osterhaus, Research Center for Emerging Infections and Zoonoses, University of Veterinary Medicine Hannover, Buenteweg 17, 30559 Hannover, Germany
Top