Volume 27, Number 5—May 2021
Synopsis
SARS-CoV-2 in Nursing Homes after 3 Months of Serial, Facilitywide Point Prevalence Testing, Connecticut, USA
Figure 1
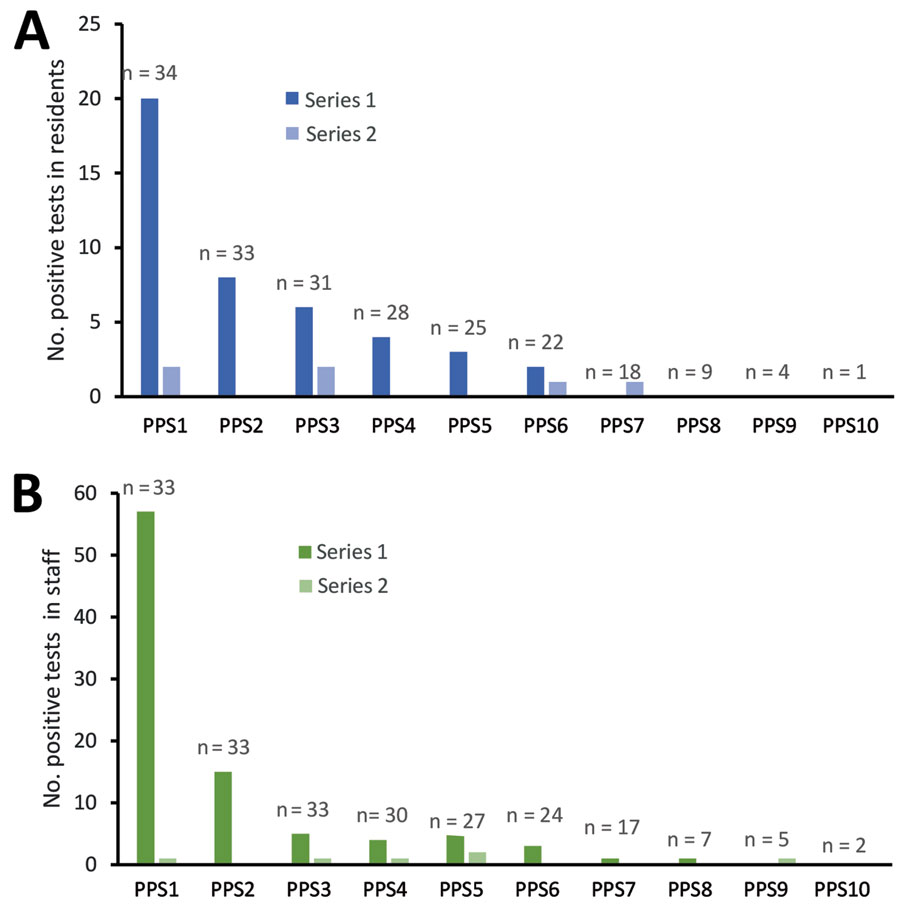
Figure 1. Coronavirus disease cases detected in consecutive PPSs in residents (A) and staff (B) in nursing homes, Connecticut, USA. The number of participating nursing homes for each survey is listed above each bar. One facility was excluded from staff testing data due to lack of verifiable testing results during PPS surveys. The results of the first PPS in residents, in which 601 cases were detected, were previously reported in (6). The probability of detecting a positive case decreased significantly (p<0.05) through PPS7 for residents and PPS8 for staff, compared with the first PPS, using logistic regression for comparisons. PPS, point prevalence survey.
References
- Ouslander JG, Grabowski DC. COVID-19 in nursing homes: calming the perfect storm. J Am Geriatr Soc. 2020;68:2153–62. DOIPubMedGoogle Scholar
- Barnett ML, Grabowski DC. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1:
e200369 . DOIGoogle Scholar - Danis K, Fonteneau L, Georges S, Daniau C, Bernard-Stoecklin S, Domegan L, et al.; ECDC Public Health Emergency Team. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. Euro Surveill. 2020;25:
2000956 .PubMedGoogle Scholar - Louie JK, Scott HM, DuBois A, Sturtz N, Lu W, Stoltey J, et al.; San Francisco Department of Public Health COVID-19 Skilled Nursing Facility Outbreak Response Team. Lessons from mass-testing for COVID-19 in long term-care facilities for the elderly in San Francisco. Clin Infect Dis. 2020;•••:
ciaa1020 . DOIPubMedGoogle Scholar - Marossy A, Rakowicz S, Bhan A, Noon S, Rees A, Virk M, et al. A study of universal severe acute respiratory syndrome coronavirus 2 RNA testing of residents and staff in a large group of care homes in South London. J Infect Dis. 2021;223:381–8. DOIPubMedGoogle Scholar
- Parikh S, O’Laughlin K, Ehrlich HY, Campbell L, Harizaj A, Durante A, et al. Point prevalence testing of residents for SARS-CoV-2 in a subset of Connecticut nursing homes. JAMA. 2020;324:1101–3. DOIPubMedGoogle Scholar
- Dora AV, Winnett A, Jatt LP, Davar K, Watanabe M, Sohn L, et al. Universal and serial laboratory testing for SARS-CoV-2 at a long-term care skilled nursing facility for veterans—Los Angeles, California, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:651–5. DOIPubMedGoogle Scholar
- Hatfield KM, Reddy SC, Forsberg K, Korhonen L, Garner K, Gulley T, et al. Facility-wide testing for SARS-CoV-2 in nursing homes—seven US jurisdictions, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1095–9. DOIPubMedGoogle Scholar
- Njuguna H, Wallace M, Simonson S, Tobolowsky FA, James AE, Bordelon K, et al. Serial laboratory testing for SARS-CoV-2 infection among incarcerated and detained persons in a correctional and detention facility—Louisiana, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:836–40. DOIPubMedGoogle Scholar
- Birgand G, Blanckaert K, Deschanvres C, Vaudron A, Loury P, King L; Group for Covid-19 control in Vendée. Testing strategies for the control of COVID-19 in nursing homes: Universal or targeted screening? J Infect. 2021;82:159–98. DOIPubMedGoogle Scholar
- Lamont N. Executive order No. 7UU:protection of public health and safety during COVID-19 pandemic and response – staff testing for nursing homes and assisted living; definition of suitable work. June 1, 2020 [cited 2020 Aug 11]. https://portal.ct.gov/-/media/Office-of-the-Governor/Executive-Orders/Lamont-Executive-Orders/Executive-Order-No-7UU.pdf
- Coleman-Mitchell RD. COVID-19 point prevalence survey testing and cohorting in nursing homes [interim guidance – May 11, 2020]. State of Connecticut Department of Public Health. May 11, 2020 [cited 2020 Aug 11]. https://www.mutualaidplan.org/Common/Document.aspx?DDID=17279&klv=1&key=uMyL4RqHDPX56fClceBfiW4N5MY%3D
- Centers for Disease Control and Prevention. Testing guidelines for nursing homes: interim SARS-CoV-2 testing guidelines for nursing home residents and healthcare personnel. Oct. 16, 2020 [cited 2020 Oct 20. https://www.cdc.gov/coronavirus/2019-ncov/hcp/nursing-homes-testing.html
- Centers for Disease Control and Prevention. Return to work criteria for healthcare personnel with SARS-CoV-2 infection (interim guidance). August 10, 2020 [cited 2020 Aug 11]. https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html
- Mathematica Policy Research. A study of the COVID-19 outbreak and response in Connecticut long-term care facilities: final report. September 30, 2020 [cited 2020 Oct 20]. https://portal.ct.gov/Coronavirus/Long-Term-Care-Facility-review
- State of Connecticut. Connecticut COVID-19 data tracker. 2020 [cited 2020 Oct 20]. https://portal.ct.gov/coronavirus/covid-19-data-tracker
- Connecticut Department of Public Health Annual town and county population for Connecticut. 2020 [cited 2020 Oct 20]. https://portal.ct.gov/DPH/Health-Information-Systems–Reporting/Population/Annual-Town-and-County-Population-for-Connecticut
- Eckardt P, Guran R, Hennemyre J, Arikupurathu R, Poveda J, Miller N, et al. Hospital affiliated long term care facility COVID-19 containment strategy by using prevalence testing and infection control best practices. Am J Infect Control. 2020;48:1552–5. DOIPubMedGoogle Scholar
- McBee SM, Thomasson ED, Scott MA, Reed CL, Epstein L, Atkins A, et al. Notes from the field: universal statewide laboratory testing for SARS-CoV-2 in nursing homes—West Virginia, April 21–May 8, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1177–9. DOIPubMedGoogle Scholar
- Bigelow BF, Tang O, Barshick B, Peters M, Sisson SD, Peairs KS, et al. Outcomes of universal COVID-19 testing following detection of incident cases in 11 long-term care facilities. JAMA Intern Med. 2021;181:127–9. DOIPubMedGoogle Scholar
- Escobar DJ, Lanzi M, Saberi P, Love R, Linkin DR, Kelly JJ, et al. Mitigation of a coronavirus disease 2019 outbreak in a nursing home through serial testing of residents and staff. Clin Infect Dis. 2020;
ciaa1021 ; [Epub ahead of print]. DOIGoogle Scholar - Taylor J, Carter RJ, Lehnertz N, Kazazian L, Sullivan M, Wang X, et al.; Minnesota Long-Term Care COVID-19 Response Group. Serial testing for SARS-CoV-2 and virus whole genome sequencing inform infection risk at two skilled nursing facilities with COVID-19 outbreaks—Minnesota, April–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1288–95. DOIPubMedGoogle Scholar
- Telford CT, Onwubiko U, Holland DP, Turner K, Prieto J, Smith S, et al. Preventing COVID-19 outbreaks in long-term care facilities through preemptive testing of residents and staff members—Fulton County, Georgia, March–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1296–9. DOIPubMedGoogle Scholar
- Sanchez GV, Biedron C, Fink LR, Hatfield KM, Polistico JMF, Meyer MP, et al. Initial and repeated point prevalence surveys to inform SARS-CoV-2 infection prevention in 26 skilled nursing facilities—Detroit, Michigan, March–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:882–6. DOIPubMedGoogle Scholar
- Montoya A, Jenq G, Mills JP, Beal J, Diviney Chun E, Newton D, et al. Partnering with local hospitals and public health to manage COVID-19 outbreaks in nursing homes. J Am Geriatr Soc. 2021;69:30–6. DOIPubMedGoogle Scholar
- Borras-Bermejo B, Martínez-Gómez X, San Miguel MG, Esperalba J, Antón A, Martin E, et al. Asymptomatic SARS-CoV-2 infection in nursing homes, Barcelona, Spain, April 2020. Emerg Infect Dis. 2020;26:2281–3. DOIPubMedGoogle Scholar
- He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–5. DOIPubMedGoogle Scholar
- Cevik M, Tate M, Lloyd O, Maraolo AE, Schafers J, Ho A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2021;2:E13–3E22.
- Tavoschi L, Vroling H, Madeddu G, Babudieri S, Monarca R, Vonk Noordegraaf-Schouten M, et al. Active case finding for communicable diseases in prison settings: increasing testing coverage and uptake among the prison population in the European Union/European Economic Area. Epidemiol Rev. 2018;40:105–20. DOIPubMedGoogle Scholar
- Paltiel AD, Schwartz JL, Zheng A, Walensky RP. Clinical outcomes of a COVID-19 vaccine: implementation over efficacy. Health Aff (Millwood). 2021;40:42–52. DOIPubMedGoogle Scholar
Page created: April 01, 2021
Page updated: April 20, 2021
Page reviewed: April 20, 2021
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.