Volume 28, Number 12—December 2022
Research Letter
Autochthonous Angiostrongylus cantonensis Lungworms in Urban Rats, Valencia, Spain, 2021
Cite This Article
Citation for Media
Abstract
To determine the role of rats as potential reservoirs of zoonotic parasites, we examined rats trapped in urban sewers of Valencia, Spain, in 2021. Morphologic and molecular identification and sequencing identified autochthonous Angiostrongylus cantonensis nematodes, the most common cause of human eosinophilic meningitis, in pulmonary arteries of Rattus norvegicus and R. rattus rats.
In Valencia, Spain, permanent rodent control campaigns are the responsibility of The Pest Control Section of the Health Service of Valencia City Council. As part of its tasks, the Section traps Rattus norvegicus and R. rattus rats in standard snap traps in the sewage system of Valencia. The trapped rodents were preserved in their entirety at −20°C and subsequently, to determine the potential reservoir role of zoonotic parasitic diseases, we defrosted the rats and analyzed the endoparasites.
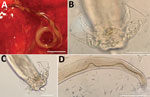
In 2021, we collected 29 adult A. cantonensis nematodes (21 female and 8 male) from the organs of the first 27 trapped rats (25 R. norvegicus and 2 R. rattus) under a stereomicroscope once the rats had been dissected. The nematodes were detected in the pulmonary arteries of 2 R. norvegicus rats and 1 R. rattus rat; 7 young nematode adults were also found in the brain of the same R. rattus rat. Adult females showed the typical barber pole spiral of lungworms of the genus Angiostrongylus (Figure, panel A). After clarifying adult male worms with Amman’s lactophenol and studying their morphology (Figure, panels B–D), we found that the measurements were consistent with rat lungworm species of A. cantonensis (Table) (1,2).
The parasite morphology, its microhabitat, and the nature of the definitive hosts clearly suggested that the parasites were A. cantonensis. To confirm species identification, we isolated total genomic DNA by using the DNeasy Blood and Tissue kit (QIAGEN, https://www.qiagen.com) according to the manufacturer’s instructions. We confirmed nematode species identity by PCR and sequencing of the cytochrome c oxidase subunit 1 (3); all sequences obtained were clustered with A. cantonensis. The phylogenetic tree grouped the A. cantonensis lungworms from Valencia close to the published sequences MK570629 and MN227185, corresponding to A. cantonensis lungworms isolated from Tenerife and Mallorca, respectively (Appendix Figure 1). We submitted the sequences we obtained to GenBank (accession no. ON819883 for the female specimen and ON819884 for the male). Likewise, when we sequenced the second internal transcribed spacer region, we found that our specimens formed a clade that differed from the other species of Angiostrongylus (Appendix Figure 2). We also submitted those sequences to GenBank (accession no. OM829831 for the male specimen and OM829832 for the female).
Male and female adult A. cantonensis lungworms live in the pulmonary arteries of Rattus rats, their preferred definitive hosts (4). Intermediate hosts are terrestrial or freshwater mollusks, such as snails and slugs. The female worms lay eggs, which give rise to L1 larvae that penetrate the alveolae and are swallowed by the rat and shed in the feces. After ingestion by an intermediate host, L1 larvae molt into L3 larvae. When infected mollusks are ingested by a rat, the subsequent phase takes place in the rat brain, where L3 larvae turn into young adults (L5). After leaving the central nervous system, L5 young adult worms reach the pulmonary arteries, where they mature and reproduce. Paratenic hosts include crabs, shrimp, frogs, and lizards (4).
Angiostrongyliasis is a foodborne disease; therefore, human infection requires ingestion of raw/poorly cooked intermediate or paratenic hosts. Another source of infection is lettuce contaminated with infective larvae released by an intermediate host (5). Hence, when humans accidentally ingest L3 larvae, the larvae penetrate the intestinal wall and travel through the bloodstream to the brain, where they can cause acute eosinophilic meningitis (neuroangiostrongyliasis). Severe cases can result in radiculitis, cranial neuropathy, myelitis, encephalopathy, coma, and even death. Usually, the nematodes die in the central nervous system (6).
Neuroangiostrongyliasis is a global emerging disease with serious implications for animal and public health (4). Globalization has helped disperse, and probably continues to disperse, rat lungworms. Infected rats (and snails) travel by ship, thereby transferring the parasite between continents and countries (7). Infected rats have been found near the port of Valencia but also several kilometers from the coast, suggesting a wide distribution of the rat lungworm in the city (Appendix Figure 3).
A. cantonensis lungworms have been reported widely in Asia, Africa, and America. However, in Europe, they have thus far been reported exclusively at the insular level, specifically in R. norvegicus and R. rattus rats in Tenerife (Canary Islands) and in Atelerix algirus hedgehogs in Mallorca (Balearic Islands) (2,8,9). Although a possible autochthonous human case of A. cantonensis infection was (immunologically) diagnosed in France, the possibility of its being an imported case was not ruled out (10).
A. cantonensis lungworms, a dangerous invasive species, agents of a potentially fatal emerging infectious disease, are spreading into locations beyond their typical tropical/subtropical distribution, probably favored not only by globalization but also by climate change. Epidemiologic surveys of rat populations in Europe, preferably in urban/peri-urban areas, with the involvement of government entities, pest control agencies, and experts in parasitic zoonoses, should help minimize future potential human infections.
Prof. Galán-Puchades is director of the Research Group on Parasites and Health of the University of Valencia. Her research interests include neglected parasitic diseases.
Acknowledgment
We thank the Health Service of Valencia City Council for overseeing and promoting this research in the city.
References
- Yousif F, Ibrahim A. The first record of Angiostrongylus cantonensis from Egypt. Z Parasitenkd. 1978;56:73–80. DOIPubMedGoogle Scholar
- Foronda P, López-González M, Miquel J, Torres J, Segovia M, Abreu-Acosta N, et al. Finding of Parastrongylus cantonensis (Chen, 1935) in Rattus rattus in Tenerife, Canary Islands (Spain). Acta Trop. 2010;114:123–7. DOIPubMedGoogle Scholar
- Rodpai R, Intapan PM, Thanchomnang T, Sanpool O, Sadaow L, Laymanivong S, et al. Angiostrongylus cantonensis and A. malaysiensis broadly overlap in Thailand, Lao PDR, Cambodia and Myanmar: a molecular survey of larvae in land snails. PLoS One. 2016;11:
e0161128 . DOIPubMedGoogle Scholar - Barratt J, Chan D, Sandaradura I, Malik R, Spielman D, Lee R, et al. Angiostrongylus cantonensis: a review of its distribution, molecular biology and clinical significance as a human pathogen. Parasitology. 2016;143:1087–118. DOIPubMedGoogle Scholar
- Waugh CA, Shafir S, Wise M, Robinson RD, Eberhard ML, Lindo JF. Human Angiostrongylus cantonensis, Jamaica. Emerg Infect Dis. 2005;11:1977–8. DOIPubMedGoogle Scholar
- Johnston DI, Dixon MC, Elm JL, Calimlim PS, Sciulli RH, Park SY. Review of cases of angiostrongyliasis in Hawaii, 2007-2017. Am J Trop Med Hyg. 2019;101:608–16. DOIPubMedGoogle Scholar
- Hochberg NS, Blackburn BG, Park SY, Sejvar JJ, Effler PV, Herwaldt BL. Eosinophilic meningitis attributable to Angiostrongylus cantonensis infection in Hawaii: clinical characteristics and potential exposures. Am J Trop Med Hyg. 2011;85:685–90. DOIPubMedGoogle Scholar
- Martín-Carrillo N, Feliu C, Abreu-Acosta N, Izquierdo-Rodriguez E, Dorta-Guerra R, Miquel J, et al. A peculiar distribution of the emerging nematode Angiostrongylus cantonensis in the Canary Islands (Spain): recent introduction or isolation effect? Animals (Basel). 2021;11:1267. DOIPubMedGoogle Scholar
- Paredes-Esquivel C, Sola J, Delgado-Serra S, Puig Riera M, Negre N, Miranda MA, et al. Angiostrongylus cantonensis in North African hedgehogs as vertebrate hosts, Mallorca, Spain, October 2018. Euro Surveill. 2019;24:
1900489 . DOIPubMedGoogle Scholar - Nguyen Y, Rossi B, Argy N, Baker C, Nickel B, Marti H, et al. Autochthonous case of eosinophilic meningitis caused by Angiostrongylus cantonensis, France, 2016. Emerg Infect Dis. 2017;23:1045–6. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleOriginal Publication Date: November 10, 2022
1These first authors contributed equally to this article.
Table of Contents – Volume 28, Number 12—December 2022
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
María Teresa Galán-Puchades, Department of Pharmacy, Pharmaceutical Technology and Parasitology, Faculty of Pharmacy, University of Valencia Av. Vicent Andrés Estellés s/n, 46100 Burjassot-Valencia, Spain
Top