Volume 30, Number 1—January 2024
Research Letter
Frequency of Children Diagnosed with Perinatal Hepatitis C, United States, 2018–2020
Cite This Article
Citation for Media
Abstract
We describe hepatitis C testing of 47 (2%) of 2,266 children diagnosed with perinatal hepatitis C who were exposed during 2018–2020 in 7 jurisdictions in the United States. Expected frequency of perinatal transmission is 5.8%, indicating only one third of the cases in this cohort were reported to public health authorities.
Hepatitis C virus (HCV) can be transmitted perinatally (1). Rates of acute HCV infection have increased recently (2), but few children perinatally exposed to HCV are tested and referred to care (3). As of November 2023, the Centers for Disease Control and Prevention recommends testing of all perinatally exposed infants for detection of HCV RNA at age 2–6 months, which is earlier than previous recommendations of ≥18 months of age for HCV antibody testing (4). There may be advantages to performing HCV RNA testing earlier, before children might become lost to follow-up (5). A prior analysis found only 16% of children perinatally exposed to hepatitis C in Philadelphia, Pennsylvania, USA, received HCV testing (6). Limited data are available from larger surveillance cohorts about current testing patterns of children perinatally exposed to HCV.
Positive HCV test results are nationally notifiable in the United States, but negative HCV test results are not. To identify potential gaps in testing and surveillance, we used positive HCV test results to describe testing and frequency of children diagnosed with perinatal hepatitis C during 2018–2020 compared with the expected frequency of perinatal transmission in 7 US jurisdictions. This activity was deemed as public health surveillance and not research at Centers for Disease Control and Prevention, thus exempt from institutional review board review.
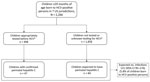
We assembled a retrospective cohort from surveillance data of pregnant women. The exposure of interest was prenatal exposure to HCV, and perinatal hepatitis C was the outcome. The Surveillance for Emerging Threats to Pregnant People and Infants Network conducts surveillance of pregnant women with HCV infection and their children (7). As of September 9, 2022, seven US jurisdictions (Georgia, Los Angeles County, Massachusetts, New York City, New York State, Pennsylvania, Tennessee) had contributed data on persons with HCV RNA detected during or within 1 year before pregnancy who had no evidence of treatment or clearance and who had live births during January 1, 2018–October 9, 2020. Children were determined to have perinatal hepatitis C if HCV RNA was detected or they had a reactive HCV antibody test during the recommended window (RNA at ≥2 months of age or antibody at ≥18 months of age) (4). Collection of data is ongoing to provide a complete picture of testing practices, including distinguishing those who were not tested from those who tested negative. We determined the expected number of children with perinatal hepatitis C by estimating 5.8% (95% CI 4.2%–7.8%) of live births exposed to HCV from included jurisdictions on the basis of a published estimate (1).
A total of 2,266 children were born to pregnant women with hepatitis C during the surveillance period (Figure). Among those children, 408 (18%) were tested for HCV infection within the recommended window and 19 (1%) outside it. Forty-seven children (2%) had perinatal hepatitis C. Median age at initial positive test was 18.6 months. Perinatal HCV infection was detected at <18 months of age for 17 (36%) children and ≥18 months of age for 30 (64%) (Table). Of the 47 children with perinatal hepatitis C, 18 (38%) had a reactive HCV antibody test and HCV RNA detected on the same day, likely reflecting reflex laboratory testing.
The expected number (1) of children with perinatal hepatitis C by 20 months of age was 131 (95% CI 95–176), suggesting there were an additional 84 children with unidentified perinatal hepatitis C in this cohort. Therefore, only 36% (47/131) of children by 20 months of age who were expected to have perinatal hepatitis C within our cohort were reported to public health authorities. Potential reasons for this discrepancy include loss to follow-up (e.g., patients did not attend follow-up appointments), lack of awareness of the need for testing, delayed testing or testing too early, not completing ordered tests (8), or lack of reporting positive tests to health departments.
Limitations of this report include the fact that negative tests are not uniformly reportable across the jurisdictions we studied. However, medical record abstraction is ongoing to be able to describe testing practices, including those who were not tested or tested negative. In addition, the number of children included in this analysis may be underestimated if confirmatory testing occurred outside of the jurisdiction for the pregnant person or they were lost to follow-up before delivery. Last, although 5.8% is a pooled estimate for risk of vertical HCV infection, underlying differences between the prior study population and the population included in this analysis could affect risk (1).
This report identified more positive infants than a previous study (36% vs. 16%) (6), but both indicate that most children perinatally exposed to hepatitis C are not tested for infection. Understanding testing patterns among children with perinatal HCV exposure and current gaps in perinatal HCV testing and surveillance will help serve as a baseline for improving testing and surveillance to identify children with perinatal hepatitis C, connect them to the appropriate care, and move toward hepatitis C elimination.
Ms. Newton is an epidemiologist with the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, Atlanta, Georgia. Her main areas of study include infections during pregnancy and short- and long-term impact to the child.
Acknowledgments
We acknowledge the following persons and organizations for their contributions to this report: Laura Price, Tennessee Department of Health; Cynthia Brooks, Chickasaw Nation Industries; Hanna Shephard, Susan Soliva, Mahsa M. Yazdy, and Catherine M. Brown, Massachusetts Department of Public Health; Katherine Barter, Allison Longenberger, and Sharon Watkins, Pennsylvania Department of Health; Allegheny County Health Department; J. Michael Bryan, Jerusha Barton, Teri Willabus, Victoria Sanon, Michael Andrews, Nehali Shah, Tracy Kavanaugh, and Ami Gandhi, Georgia Department of Public Health; Prabhu Gounder, Raiza Amiling, Bonnie Dao, Nina Mykhaylov, Van Ngo, and Clara Chang, Los Angeles County Department of Health; and Lucila Zamboni, New York State Department of Health.
This study was performed as regular work of the Centers for Disease Control and Prevention. This work is supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement (CK19-1904) and contractual mechanisms, including the Local Health Department Initiative to Chickasaw Health Consulting (200-2021-F-12655). Staffing support for this work was funded by CDC to a contract to Eagle Global Scientific (200-2019-06754).
References
- Benova L, Mohamoud YA, Calvert C, Abu-Raddad LJ. Vertical transmission of hepatitis C virus: systematic review and meta-analysis. Clin Infect Dis. 2014;59:765–73. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Viral hepatitis surveillance report—United States, 2020. 2022 Sep [cited 2022 Nov 8]. https://www.cdc.gov/hepatitis/statistics/2020surveillance/index.htm
- Lopata SM, McNeer E, Dudley JA, Wester C, Cooper WO, Carlucci JG, et al. Hepatitis C testing among perinatally exposed infants. Pediatrics. 2020;145:
e20192482 . DOIPubMedGoogle Scholar - Panagiotakopoulos L, Sandul AL, Conners EE, Foster MA, Nelson NP, Wester C, et al.; DHSc; Collaborators. CDC recommendations for hepatitis C testing among perinatally exposed infants and children—United States, 2023. MMWR Recomm Rep. 2023;72(No. RR-4):1–21. DOIPubMedGoogle Scholar
- Bhardwaj AM, Mhanna MJ, Abughali NF. Maternal risk factors associated with inadequate testing and loss to follow-up in infants with perinatal hepatitis C virus exposure. J Neonatal Perinatal Med. 2021;14:123–9. DOIPubMedGoogle Scholar
- Kuncio DE, Newbern EC, Johnson CC, Viner KM. Failure to test and identify perinatally infected children born to hepatitis C virus–infected women. Clin Infect Dis. 2016;62:980–5. DOIPubMedGoogle Scholar
- Woodworth KR, Reynolds MR, Burkel V, Gates C, Eckert V, McDermott C, et al. A preparedness model for mother-baby linked longitudinal surveillance for emerging threats. Matern Child Health J. 2021;25:198–206. DOIPubMedGoogle Scholar
- Reynolds B. Birth and infant outcomes in pregnancies affected by hepatitis C-SETNET, Allegheny County, PA. Abstract presented at: Council of State and Territorial Epidemiologists Annual Conference. June 19–23, 2022; Louisville, KY, USA.
Figure
Table
Cite This ArticleOriginal Publication Date: December 07, 2023
Table of Contents – Volume 30, Number 1—January 2024
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Address correspondence to: Suzanne M. Newton, MPH, Centers for Disease Control and Prevention, 4770 Buford Hwy, Mailstop S106-3, Atlanta, GA 30341, USA
Top