Volume 30, Number 9—September 2024
Research
Autochthonous Leishmaniasis Caused by Leishmania tropica, Identified by Using Whole-Genome Sequencing, Sri Lanka
Figure 1
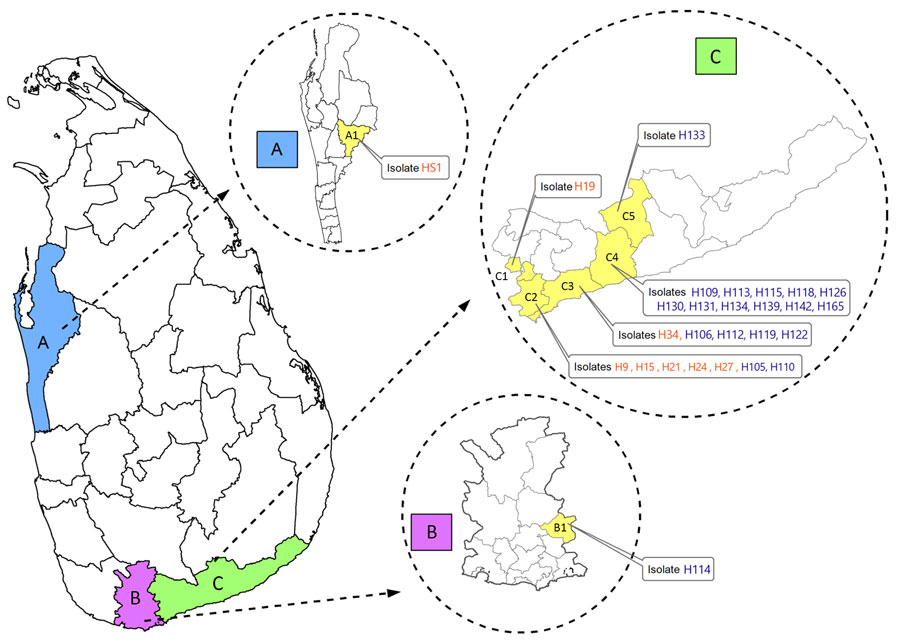
Figure 1. Geographic locations of patients with cutaneous or mucocutaneous leishmaniasis in Sri Lanka. The mucocutaneous leishmaniasis patient was from the Puttalam district (A), Anamaduwa subdistrict. The cutaneous leishmaniasis patients were from both the Matara (B) and Hambantota (C) districts. Isolates labeled in orange were identified as Leishmania tropica. Isolates labeled in blue were identified as L. donovani. A, Puttalam district; A1, Anamaduwa; B, Matara district; B1, Hakmana; C, Hambantota district; C1, Okewela; C2, Beliatta; C3, Tangalle; C4, Ambalantota; C5, Sooriyawewa.
1These authors contributed equally to this article.
Page created: August 07, 2024
Page updated: August 20, 2024
Page reviewed: August 20, 2024
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.