Volume 20, Number 7—July 2014
Letter
Zoonotic Filariasis Caused by Novel Brugia sp. Nematode, United States, 2011
Cite This Article
Citation for Media
To the Editor: Zoonotic brugian filariasis is an incidental infection of humans with Brugia spp. nematodes that primarily parasitize nonhuman vertebrates, rarely humans (1–3). In contrast to classical lymphatic filariasis caused by B. malayi and B. timori, which are found in Asia, most zoonotic Brugia infections have been reported from the northeastern United States (2,3) or South America (3). We report a case of symptomatic brugian infection in a New York City resident who had not traveled to the Eastern Hemisphere.
In 2011, a 53-year-old White man first noted tenderness and swelling behind his penis and in his right groin after having fallen 3 months earlier. The tenderness was relieved by nonsteroidal antiinflammatory drugs, but the swelling continued; an oral antimicrobial drug, prescribed for presumed cellulitis, produced no improvement. At the time of examination, the patient had no fever or other signs or symptoms. Only a 3.0-cm × 3.0-cm firm, nonfixed right inguinal nodule without warmth or tenderness was noted. Laboratory findings were remarkable for total leukocytes of 6.4 × 109, eosinophilia (12%, 600 cells/mm3), decreased hemoglobin level (10.0 g/dL), and low hematocrit of 31.2%. An excisional biopsy sample revealed intralymphatic adult nematodes with viable-appearing microfilaria (Technical Appendix Figure).
The patient had been born and raised in Champlain, Illinois, and had resided in the Bronx, New York, since 1979; he had no history of travel to filariasis-endemic regions. Characteristics of the adult worms and microfilaria were most consistent with those of Brugia spp., which was surprising because classical brugian lymphatic filariasis seems to be limited to Asia (B. malayi) and Indonesia (B. timori) (4,5). However, the adult filariae were smaller than expected for B. malayi or B. timori nematodes, prompting consideration of zoonotic filariasis (1,6). The adult worms and microfilaria seemed to be viable, although zoonotic Brugia spp. in histologic sections often appear degenerated (1,2,6). The diameters of the adult worms were similar to those reported from South America (females 90–100 μm, males 50 μm) (7,8) rather than those from North America (females 35–75 μm, males 32–52 μm) (1). Peripheral blood was repeatedly negative for microfilaria. Serum sent to the Centers for Disease Control and Prevention (Atlanta, GA, USA) for ELISA testing for B. malayi anti-filarial IgG 4 showed optical density of 0.13, below the ELISA cutoff for filariasis.
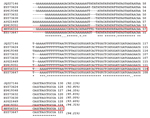
Because micromorphologic information was not adequate for species identification, paraffin-embedded biopsy specimens were submitted for molecular testing. Genomic DNA extracted from paraffin-embedded tissue with the QIAamp DNA–formalin-fixed, paraffin-embedded tissue procedure was amplified by using the primer sets DiBu-F(5′-GCTAGATATGCTACCAACAAAA-3′)/ITS1 R(5′-CTCAATGCGTCTGCAATTCGC-3′) and BuF2-(5-CATTTATGCTAGATATGCTACCAAC-3′)/ITS1-R. The products were fractionated on 2% agarose gel and stained with ethidium bromide. The internal transcribed spacer (ITS) 1 PCR product (182 bp) was automatically sequenced by using the same primers used for PCR. Lasergene software (DNASTAR, Madison, WI, USA) was used to align the sequences obtained with Brugia spp. sequences deposited in GenBank; detailed sequence comparison identified the isolate as a novel Brugia (Nematoda: Onchocercidae) species closely related to B. pahangi and B. malayi (Figure). The ITS-1 sequence was submitted to the EMBL Nucleotide Sequence Database (accession no. HE856316).
Removal of an affected lymph node without additional treatment is often considered sufficient treatment for zoonotic filariases. However, for the patient reported here, persistence of inguinal swelling prompted a repeat biopsy 4 months later; the specimen again demonstrated reactive follicular hyperplasia, although no parasites were seen. Because the patient’s initial clinical signs and subsequent persistent adenopathy were reminiscent of unilateral lymphadenitis, lymphangitis, and induration that are typical of B. malayi or B. timori filariasis, and the microfilariae in the original biopsy sample appeared to be viable, we empiricially prescribed a standard dosage of oral doxycycline for 6 weeks, followed by single doses of ivermectin at 400 μg/kg and 800 mg albendazole. The patient has been well, without further adenopathy or eosinophilia, for >2 years. Because adult filariae can live for >10 years, the place of acquisition cannot be stated with certainty.
The prevalence of zoonotic infection with Brugia spp. nematodes is unknown. Many reported cases are asymptomatic or diagnosed incidentally during evaluation for persistent adenopathy (1–3). Conversely, differentiation of zoonotic from classical filariasis is unlikely in disease-endemic areas; most cases published since the initial 1962 case report (1) occurred in the United States. Most case-patients were from the Northeast, including New York (8 cases), Massachusetts, Pennsylvania, Connecticut, and Rhode Island (3 cases each) (1,2); single cases have been identified in Michigan, Ohio, North Carolina, Oklahoma, New Jersey, Louisiana, Florida, and California (1,2). Four other cases have been reported: 3 in South America (Colombia, Brazil, Peru) (3,7,8) and 1 in Africa (Ethiopia) (9). Only a few Brugia species have been identified, including B. leporis, found in rabbits in the northeastern United States (1,10); B. beaveri, found in raccoons and bobcats in the southern United States; and B. guyanensis, found in coatimundi and other vertebrates in South America (8). Definitive identification with molecular techniques will better identify causative species and help clarify many of the ecologic and epidemiologic questions surrounding zoonotic filarial infections.
Acknowledgment
This work was supported by the Instituto de Salud Carlos III, Fondo de Investigaciónes Sanitarias, through the sixth national plan of research plus development plus innovation (2008–2011), Instituto de Salud Carlos III -General Sub-Direction of Networks and Centers for Collaborative Research (Red Temática de Investigación Cooperativa–Red de Investigación Cooperativa en Enfermedades Tropicales, grant no. RD12/0018/003).
References
- Orihel TC, Eberhard ML. Zoonotic filariasis. Clin Microbiol Rev. 1998;11:366–81 .PubMedGoogle Scholar
- Eberhard ML, DeMeester LJ, Martin BW, Lammie PJ. Zoonotic Brugia infection in western Michigan. Am J Surg Pathol. 1993;17:1058–61 . DOIPubMedGoogle Scholar
- Orihel TC, Beaver PC. Zoonotic Brugia infections in North and South America. Am J Trop Med Hyg. 1989;40:638–47 .PubMedGoogle Scholar
- Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet. 2010;376:1175–85. DOIPubMedGoogle Scholar
- Schneider MC, Aguilera XP, Barbosa da Silva Junior J, Ault SK, Najera P, Martinez J, Elimination of neglected diseases in Latin America and the Caribbean: a mapping of selected diseases. PLoS Negl Trop Dis. 2011;5:e964. DOIPubMedGoogle Scholar
- Gutierrez Y. Diagnostic features of zoonotic filariae in tissue sections. Hum Pathol. 1984;15:514–25. DOIPubMedGoogle Scholar
- Kozek WJ, Reyes MA, Ehrman J, Garrido F, Nieto M. Enzootic Brugia infection in a two-year old Colombian girl. Am J Trop Med Hyg. 1984;33:65–9 .PubMedGoogle Scholar
- Baird JK, Neafie RC. South American brugian filariasis: report of a human infection acquired in Peru. Am J Trop Med Hyg. 1988;39:185–8 .PubMedGoogle Scholar
- Menéndez MC, Bouza M. Brugia species in a man from western Ethiopia. Am J Trop Med Hyg. 1988;39:189–90 .PubMedGoogle Scholar
- Beaver PC, Orihel TC. Human infection with filariae of animals in the United States. Am J Trop Med Hyg. 1965;14:1010–29 .PubMedGoogle Scholar
Figure
Cite This ArticleRelated Links
Table of Contents – Volume 20, Number 7—July 2014
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Alberto E. Paniz-Mondolfi, Yale–New Haven Hospital, Microbiology Laboratory (PS656), 55 Park St, New Haven, CT 06511, USA
Top