Volume 26, Number 9—September 2020
Research
No Change in Risk for Antibiotic-Resistant Salmonellosis from Beef, United States, 2002–2010
Abstract
Restricting antibiotic use in food production animals is a target for reducing antimicrobial drug–resistant infections in humans. We used US surveillance data to estimate the probability of antibiotic-resistant nontyphoidal salmonellosis per meal made with beef during 2002–2010. Applying data for nontyphoidal Salmonella in raised-without-antibiotics cattle, we tested the effect of removing antibiotic use from all beef cattle production. We found an average of 1.2 (95% credible interval 0.6–4.2) antibiotic-resistant nontyphoidal salmonellosis cases per 1 million beef meals made with beef initially contaminated with antibiotic-resistant nontyphoidal Salmonella at slaughter or retail and 0.031 (95% credible interval 0.00018–0.14) cases per 1 million meals irrespective of beef contamination status. Neither outcome showed sustained change except for increases in 2003 and 2009 (>98% confidence) when larger or more outbreaks occurred. Switching all beef production to a raised-without-antibiotics system may not have a significant effect on antibiotic-resistant nontyphoidal salmonellosis (94.3% confidence).
Increased antimicrobial resistance (AMR), or antibiotic resistance, has resulted in initiatives to reduce the use of antibiotics in food production animals (1,2), but quantification of the public health effects of decreasing antibiotic use in livestock remains limited (3,4). Reduction of antibiotic use in livestock can lower resistance prevalence (i.e., proportion of pathogens with resistance) in animals (4), but some studies show that pathogen prevalence may be higher in livestock raised without antibiotics (5). Because transmission of foodborne pathogens is proportional to the prevalence of pathogens in the food source (6), quantifying the change in human antibiotic-resistant foodborne illnesses resulting from reduced antibiotic use in livestock is vital.
In the United States, the most common bacterial cause of foodborne illness is nontyphoidal Salmonella (NTS), which leads to >1 million foodborne illnesses and 20,000 hospitalizations per year (7). Antibiotic-resistant NTS is among the top 18 AMR threats in the United States (8), causing 100,000 infections annually. The Centers for Disease Control and Prevention National Antimicrobial Resistance Monitoring System (NARMS) tracks resistance to 25 antibiotics in patient samples positive for isolates such as NTS (9), including the clinically relevant antibiotics ciprofloxacin and ceftriaxone.
Multiple assessments of human AMR risk from meats have been performed (10–14). However, most focused on only 1 class of antibiotic (10,11), had limited or no longitudinal data (14), or were not based on nationwide surveillance at the animal source (11). Quantitative assessments of AMR risk with a more comprehensive resistance definition (15), such as resistance to any class, or to >3 classes, that use representative, longitudinal data, are critical to defining the risks and benefits from policy with regard to antibiotic use in livestock (3). Surveillance studies of antibiotic use and AMR in humans and livestock can be used to generate estimates of risk based on empirical data and can show the results of long-term conditions or systematic changes over time.
Our objective with this study was to use beef as a model to quantify trends in the longitudinal relationship human NTS infections and antibiotic-resistant NTS in meats. We also used the estimates to predict change in antibiotic-resistant salmonellosis resulting from hypothetical scenarios of antibiotic restriction in beef cattle.
We developed a stochastic model to quantify the risk for antibiotic-resistant nontyphoidal salmonellosis per meal made with beef during 2002–2010. Our model follows the method of previously published AMR risk assessments (6,16) but uniquely addresses temporal changes and relies solely on nationwide surveillance data (Appendix Table 1). We used this model for 3 objectives: 1) estimate the risk for antibiotic-resistant nontyphoidal salmonellosis per meal made with beef, using the yearly cases of illnesses (Illres) and the number of meals made with beef that year (Mealres) (Figure 1); 2) evaluate change over time in all model outcomes; and 3) assess the effect that potential future restrictions on antibiotic use in beef cattle would have on antibiotic-resistant nontyphoidal salmonellosis disease burden (Appendix).
Risk for Antibiotic-Resistant Nontyphoidal Salmonellosis Attributable to Beef
Annual Incidence of Beef-Attributable Antibiotic-Resistant Nontyphoidal Salmonellosis (Illres Incidence) per 100,000 Persons
We obtained the annual total nontyphoidal salmonellosis cases in the United States for 1998–2015 from FoodNet (https://www.cdc.gov/foodnet), an active foodborne disease surveillance system, after adjusting for the proportion of the US population included in FoodNet surveillance sites. To correct for underdiagnosis and restrict case estimates to domestically acquired foodborne cases, we also included adjustment factors constant for the study period. By using annual food attribution estimates derived from the National Outbreak Reporting System (NORS; https://www.cdc.gov/nors/index.html), cases of nontyphoidal salmonellosis were further restricted to foodborne cases attributed to ground beef and intact beef. To ensure that the resistance fraction is specific to nontyphoidal salmonellosis attributed to consumption of beef, we estimated the fraction of beef-attributed nontyphoidal salmonellosis cases with AMR by matching cases in the Centers for Disease Control and Prevention data collected from clinical patient samples as part of NARMS (17) with beef-attributable outbreak data from NORS by using sample metadata, (Appendix Table 1). We calculated the yearly incidence of Illres per 100,000 persons in the United States and used this outcome for trend tests.
Annual Meals Prepared with Beef Initially Contaminated with Antibiotic-Resistant NTS (Mealsres)
We calculated the number of beef meals consumed annually in the United States by using beef disappearance data from the US Department of Agriculture (USDA) (18) and the mean grams of beef consumed per beef meal from the National Health and Nutrition Examination Survey (19). We estimated the prevalence of NTS in beef by using USDA Food Safety and Inspection Service surveillance data, and we derived the fraction of isolates with AMR from USDA NARMS and US Food and Drug Administration NARMS data (9). Mealsres were stratified by beef cut (ground beef data for 2002–2015 vs. intact beef for 1998–2010). By using Mealsres, we assumed that the beef used to prepare a meal was initially contaminated (as measured at the slaughter plant or retail) with the pathogen. This assumption does not necessarily mean that the actual meal consumed was contaminated because safe cooking and handling practices would reduce or completely inactivate the bacterial load.
Risk for Antibiotic-Resistant Nontyphoidal Salmonellosis per Beef Meal
Dividing Illres by Mealsres resulted in the probability of antibiotic-resistant nontyphoidal salmonellosis per meal made with beef initially contaminated with antibiotic-resistant NTS (Pill). Also, by using all meals in the denominator, we calculated the probability of antibiotic-resistant nontyphoidal salmonellosis per meal made with beef, regardless of contamination status (Pmeal) (Figure 1). We report both risk outcomes per 1 million meals, on a per-year basis (Pill and Pmeal) and as the mean of each for all years combined (Pill,overall and Pmeal,overall). We repeated the analyses for NTS with multidrug resistance (NTSMDR) (i.e., resistance to >3 antimicrobial classes) and for clinically relevant resistance (NTSCRR), also known as resistance of concern (i.e., resistance to >5 drugs or quinolones [ciprofloxacin] or third-generation cephalosporins [ceftriaxone]) (8).
Testing for Temporal Changes
To identify the confidence of a consistent increase (or decrease) in each outcome over the study period, we used Mann-Kendall trend test bootstrapping (20). In addition, used numerical integration to compute the confidence in pairwise year-to-year Bayesian posterior differences (21) and the difference between the mean of each outcome in the last years of the study period versus the remaining previous years. Unlike the Mann-Kendall tests, the year-to-year test identified short-term changes, and the comparison of the first versus the last 5 years of the study period provided an assessment of nonlinear changes during the study period.
Scenario Analysis: Effects of Hypothetical Antibiotic Restriction in Beef Production
Relationship between Antibiotic Use and Antibiotic-Resistant NTS in Beef
To model the relationship between antibiotic use and antibiotic-resistant NTS, we used nationwide data (C.P. Fossler, USDA, pers. comm., 2018 Jul 16) from the National Animal Health Monitoring System feedlot survey (22). The feedlot survey is based on a nationwide representative sample of farms and thus captures the effect of long-term and current antibiotic practices on AMR. In the survey, individual fecal pats from raised-without-antibiotics cattle and conventionally raised cattle were collected to estimate the prevalence of NTS isolates and the fraction of these with AMR. These 2 parameters were combined to measure the overall prevalence of antibiotic-resistant NTS in raised-without-antibiotics cattle and conventionally raised cattle and to derive the relative risk (RR) of antibiotic-resistant NTS prevalence in raised-without-antibiotics versus conventionally raised cattle.
Prediction of Changes in Beef-Attributable Antibiotic-Resistant Nontyphoidal Salmonellosis
We constructed 2 scenarios to evaluate Illres changes from hypothetical antibiotic restriction in beef production. We assumed no changes in slaughtering, processing, consumer habits, and food preparation.
For scenario 1, we estimated the change in antibiotic-resistant nontyphoidal salmonellosis if all beef production were switched to raised-without-antibiotics by using the annual estimated Illres for 2002–2010 and the RR of antibiotic-resistant NTS prevalence in raised-without-antibiotics versus conventionally raised cattle. By doing so, we assumed that the animal-level prevalence of antibiotic-resistant NTS is proportional (but not equal to) its prevalence in meals prepared with beef and that RR has a direct linear effect on the change in Illres. This relationship is documented for food pathogens (6,23), including NTS (24), so here we assumed that it extends to antibiotic-resistant isolates.
To relax this assumption, for scenario 2, we empirically estimated the relationship between antibiotic-resistant NTS prevalence in beef and Illres via Poisson regression and used the Poisson regression to create an adjustment factor to the calculations done for scenario 1. For each scenario, we reported the posterior confidence in the change in Illres being <0 (i.e., reduction of antibiotic-resistant nontyphoidal salmonellosis) for each year of the study and for all years combined.
Model Implementation
We used R version 3.4.1 (https://www.R-project.org) to perform all analyses. We used Monte Carlo simulation to calculate the posterior uncertainty in all outcomes. Statistical significance was assessed at the 95% confidence level. We performed a sensitivity analysis of the key drivers of Pill and Pill,overall by calculating the effect that extreme values of each input had on the output means (Appendix).
Descriptive Statistics of Main Parameters and Risk Measures
During 2002–2010, approximately 554 billion beef meals were consumed, 59% as ground beef. Of these meals, 4% came from beef at slaughter or retail with NTS, half of which were antibiotic-resistant (11.23 billion, 95% CrI 9.08–13.54 billion). Approximately 93% of meals with beef initially contaminated with antibiotic-resistant NTS were made with ground beef (10.4 billion meals, 95% CrI 8.3–12.73 billion) (Figure 2), resulting from higher prevalence of both NTS and antibiotic-resistant NTS in ground than intact beef (Table 1). Yet, the attribution of nontyphoidal salmonellosis, regardless whether antibiotic resistance, was relatively even between ground and intact beef (Figure 2). The total incidence of Illres was 0.64 (0.0036–2.75)/100,000 persons.
During 2002–2010, the mean risk for antibiotic-resistant nontyphoidal salmonellosis was 0.031 cases (95% CrI 0.00018–0.14)/1 million beef meals; intact and ground beef contributed equally to the rate (Table 1; Figure 2). The risk per million beef meals initially contaminated with NTS was 1.8 (95% CrI 0.007–8.5) overall, 1.16 (95% CrI 0.0015–5.2) for ground beef and 9.5 (95% CrI 0.03–50) for intact beef (Figure 2). The higher Pill,overall for intact beef possibly indicates a higher risk from consumption of intact beef carrying antibiotic-resistant NTS.
Tests for Temporal Changes in Main Parameters and Risk Measures
None of the tested parameters or outcomes based on a resistance definition of >1 antibiotic (i.e., Mealsres or Illres per 100,000 population [Figure 2], or Pill or Pmeal [Figure 3]) showed a sustained change (Table 2). We also observed no change when we used multidrug resistance (MDR) and clinically relevant resistance (CRR) as the definition of resistance (Table 2; Appendix Figures 5–8), except that meals made with ground beef contaminated with NTSCRR declined during 2002–2015. More differences based on the last 5 years of the study period were found. The risk for NTSMDR per 1 million meals made with ground beef initially contaminated with NTSMDR increased during 2010–2015, while the number of these meals made with NTSMDR-contaminated ground beef decreased (Table 2). In contrast, for CRR, the beef-attributable risk for CRR nontyphoidal salmonellosis was significantly lower for all beef meals initially contaminated—and ground beef specifically—in the last 5 years of data, as were both the incidence of CRR nontyphoidal salmonellosis and its risk per 1 million beef meals, overall and for intact beef (Table 2).
We found some year-to-year variations in Illres, Pill, and Pmeal but generally no yearly changes in meals made with beef initially contaminated with antibiotic-resistant NTS (Mealres). For all beef and for ground beef and intact beef individually, defining resistance as resistance to >1 antibiotic, Illres, Pill, and Pmeal were higher in 2003 and 2009 and a peak for ground beef also occurred in 2014. Mealsres showed no significant year-to-year changes for all beef cuts combined. Intact beef Mealsres had 1 peak in 2001 (100% confidence). When MDR and CRR were used as the resistance definition, only the peaks in 2003 and in 2014 remained significant. A peak in some intact beef risks and illnesses was also observed in 2000 (Table 2).
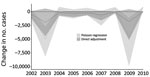
Scenario Analysis of Changes in Antibiotic-Resistant Nontyphoidal Salmonellosis Resulting from Antibiotic Restriction in Beef Production
In the first scenario analysis, we found no significant changes (<94.3% confidence) in antibiotic-resistant salmonellosis for any year when switching from current antibiotic practices to hypothetical 100% raised-without-antibiotics production. The mean change in the number of antibiotic-resistant nontyphoidal salmonellosis cases across the study period was −5,218 (Figure 4), ranging from an additional 1,441 resistant nontyphoidal salmonellosis cases to a reduction of 14,350 cases.
The second scenario (Figure 4), in which the direct linear assumption was relaxed, predicted significant decreases (>98% confidence) in cases for 2003 (−5,152) and 2009 (−4,763) and a significant increase of 1,098 cases (99.9% confidence) in 2010. However, switching to 100% raised-without-antibiotics production did not significantly change the number of antibiotic-resistant nontyphoidal salmonellosis cases over the full study period combining all 9 years (−8,588, 95% CrI −27,842 to 16,317, 60% confidence).
Our risk analysis uses nationwide surveillance data on animal production and human illnesses to longitudinally estimate antibiotic-resistant nontyphoidal salmonellosis in the United States and assess how it might be affected by antibiotic restriction in livestock. Our approach is grounded in empirical data and minimizes assumptions while modeling parameter uncertainty and its effect on the results. Although farm-to-fork AMR risk analyses have been published (10), recent work has followed more parsimonious approaches like ours (11–14). However, direct comparison with other published risk analyses is difficult because most focus on the association between antibiotic use and AMR for a single drug and rarely include longitudinal data.
In our 2002–2010 analysis, the risks were stable over time; on average, a case of antibiotic-resistant salmonellosis occurred <1 time per 32 million meals made with beef or <1 time per 500,000 meals made with beef initially contaminated with antibiotic-resistant NTS. Likewise, prevalence of the antibiotic-resistant pathogen in beef available at retail in the United States and in the food production chain remained stable. Exceptions were 2 years in which more beef-attributable illnesses occurred than was typical for other years: 5 average-sized outbreaks (8% of attributable outbreaks) in 2003 and 2 Salmonella Montevideo outbreaks with high total case numbers in 2009.
The proportion of MDR and CRR was higher in NTS isolates from NARMS matched to outbreaks in 2003 and 2009 than in other years: 80% of matched samples in 2003 had CRR, and all 2009 Salmonella Montevideo matched samples (71% of all matched 2009 cases) had MDR. This increase remained after we adjusted for exposure to infection in the form of meals prepared with beef with NTS and the fraction of these with AMR, which were stable. The association between MDR and CRR and larger/more frequent outbreaks may suggest a link between MDR/CRR and pathogenicity or infectivity, as described by Guillard et al. (25). Yet, in vitro phenotypic resistance does not fully capture actual clinical outcomes. Current foodborne surveillance programs do not record outcomes of AMR illnesses such as treatment failures and their consequences (e.g., extra hospitalizations). Estimating treatment failures resulting from resistant infections and the relative contribution of different sources of AMR—including antibiotic use in livestock—would better quantify the societal cost benefit of curtailing resistant illnesses from livestock.
In our analysis, we had to estimate AMR specific to beef-attributable cases because the NARMS database contains salmonellosis cases of any source and yet resistance of salmonella varies by source (9). Lacking direct links between the NORS outbreak data used in source attribution and the outbreaks in NARMS, we used timing of the infection, state, and serotype to match cases. Although this method enabled us to approximate resistance in beef-attributable cases (5% vs. 22% AMR across human NARMS samples for NTS over the study period), use of this method probably resulted in some misclassification of the NARMS samples. This issue would be easily alleviated if a unique outbreak identifier were available in both datasets.
Of note, the per-portion risk for susceptible or resistant salmonellosis from beef initially contaminated was »8 times higher for intact cuts of beef than for ground beef. Because the prevalence of susceptible and resistant pathogens is greater for ground beef, the total illnesses are evenly split between types of beef, as are attributed illnesses, a result also noted by Laufer et al. (26). Intact cuts include some high-risk foods such as delicatessen roast beef and ready-to-eat products (27). Doneness might also partly explain this finding. A survey found that 61% of US consumers preferred their steak medium or rarer (28), and another study found that 21% of restaurant customers requested medium or rarer hamburgers (29).
Using NTS in beef, beef-attributable salmonellosis cases, and resistance to >1 antibiotic provided a case definition that maximizes the chances of finding a statistical signal in this dataset, should a trend exist in the outcomes. Consequently, the lack of sustained change suggests that the modeled risks were indeed stable nationwide. Assuming that is often described antibiotic use in beef production is a key driver of AMR illnesses in humans, we consider 2 alternative explanations for this stability: either antibiotic use was stable during the study period or sustained use in beef resulted in a plateau in AMR salmonellosis so that changes in use can no longer affect the outcome. Although nationwide data on antibiotic use is unavailable for the study period, antibiotic use in beef is unlikely to have remained stable. For example, the fraction of beef cattle treated with tylosin in feed or water increased from 42.3% in 1999 to 71.2% in 2010 (30,31), whereas in Canada, where beef production practices are equivalent to those in the United States, overall use in beef decreased during 2008–2012 (32). A hypothetical resistance plateau cannot be empirically answered without detailed use data, but its implication is that changes such as the recent US Food and Drug Administration feed directive should eventually reduce beef-attributable antibiotic-resistant nontyphoidal salmonellosis. This hypothesis warrants a re-estimation of our model in the future.
An alternative hypothesis for the lack of change is that antibiotic use in beef does not significantly affect incidence of human AMR salmonellosis. This hypothesis does not necessarily imply a lack of risk but a risk that is too small or confounded to be measured. Empirical data for this effect are scarce because field studies typically link antibiotic use to AMR in animals or animal products, not in human illnesses. Benedict et al. (33) described how exposure to antibiotics in feedlot cattle did not affect AMR presence in non–type-specific Escherichia coli. Others have described a lower prevalence of resistance resulting from decreased use (4), although pathogen prevalence among raised-without-antibiotics livestock may be higher than that among conventionally raised animals (5). Although our study cannot confirm or refute this hypothesis, it provides new empirical evidence based on nationwide estimates and can be further updated as antibiotic practices in livestock are documented.
The scenarios with all raised-without-antibiotics beef cattle enabled us to model a hypothetical upper limit of the human health effect of antibiotic reduction and resulted in nonsignificant changes in resistant illnesses overall. This finding held true even under an unrealistic assumption of a direct decrease in resistant illnesses resulting from decreased pathogen prevalence and resistance after complete withdrawal of antibiotics. Being based solely on nationwide estimates—resistant illnesses based on surveillance data and the effect of antibiotic use on antibiotic-resistant NTS based on a nationwide survey (22)—these findings suggest that, according to collected surveillance data, reducing antibiotic use in cattle may not significantly reduce antibiotic-resistant nontyphoidal salmonellosis by a measurable level. Although external validation is not feasible because no other study, to our knowledge, has directly tested human and animal resistance at a national level, these results are consistent with those of recent studies of cecal contents of fed cattle (5) and ground beef (34) that found few AMR differences between raised-without-antibiotics and conventionally raised cattle production. Our findings also demonstrate that a direct relationship between prevalence of antibiotic-resistant NTS in beef and resulting AMR salmonellosis is not supported by current surveillance data.
This analysis suggests that the risk of contracting antibiotic-resistant nontyphoidal salmonellosis from beef consumption is <1 time/32 million beef meals and remained stable during 2002–2010. Despite assessing salmonellosis only, our work highlights improvements needed to better quantify the effect that antibiotic use in livestock has on human health: monitoring of clinical outcomes in foodborne surveillance programs, better connection between surveillance for foodborne pathogen resistance and outbreak sourcing, and detailed studies exploring the effect of raised-without-antibiotics production practices on pathogen prevalence and resistance throughout the farm-to-fork production chain. Elucidating not only consumers’ exposure to resistant pathogens but also how exposure translates into resistant illnesses and, ultimately, treatment failures, is required for the development of optimal AMR reduction strategies.
Dr. Costard is an epidemiologist working as a senior consultant at EpiX Analytics in Fort Collins, CO, USA. Her research interests include risk analysis, simulation modeling, and quantitative decision-support tools in general, with special interests in health risk management strategies and food safety.
Acknowledgments
We thank Michael D. Apley for his constructive feedback on the model and interpretation of results.
K.E.B., P.S.M., J.W.S., T.L.W., T.M.A. contributed to the study design and manuscript review and editing.
This work was supported by a research contract from the Beef Checkoff. The funders had no role in the study design, data collection or analysis, manuscript preparation, nor the decision to publish this work.
USDA is an equal opportunity provider and employer. Names are necessary to report factually on available data; however, the USDA neither guarantees nor warrants the standard of product, and use of the name by the USDA implies no approval of the product to the exclusion of others that may also be suitable.
References
- European Commission. Regulation (EC) no. 1831/2003 of the European Parliament and of the Council of 22 September 2003 on additives for the use in food and nutrition [cited 2019 Mar 4]. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32003R1831&from=EN
- Office of Information and Regulatory Affairs. Veterinary feed directive [cited 2018 Oct 18]. https://www.reginfo.gov/public/do/eAgendaViewRule?pubId=201404&RIN=0910-AG95.
- Landers TF, Cohen B, Wittum TE, Larson EL. A review of antibiotic use in food animals: perspective, policy, and potential. Public Health Rep. 2012;127:4–22. DOIPubMedGoogle Scholar
- Tang KL, Caffrey NP, Nóbrega DB, Cork SC, Ronksley PE, Barkema HW, et al. Restricting the use of antibiotics in food-producing animals and its associations with antibiotic resistance in food-producing animals and human beings: a systematic review and meta-analysis. Lancet Planet Health. 2017;1:e316–27. DOIPubMedGoogle Scholar
- Vikram A, Rovira P, Agga GE, Arthur TM, Bosilevac JM, Wheeler TL, et al. Impact of “raised without antibiotics” beef cattle production practices on occurrences of antimicrobial resistance. Appl Environ Microbiol. 2017;83:e01682–17. DOIPubMedGoogle Scholar
- Williams MS, Ebel ED, Vose D. Framework for microbial food-safety risk assessments amenable to Bayesian modeling. Risk Anal. 2011;31:548–65. DOIPubMedGoogle Scholar
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson M-A, Roy SL, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011;17:7–15. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013 [cited 2018 Dec 5]. https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf
- Centers for Disease Control and Prevention. National Antimicrobial Resistance Monitoring System (NARMS): 2014 human isolates surveillance report [cited 2018 Jan 10]. https://www.cdc.gov/narms/pdf/2014-Annual-Report-narms-508c.pdf
- Anderson SA, Yeaton Woo RW, Crawford LM. Risk assessment of the impact on human health of resistant Campylobacter jejuni from fluoroquinolone use in beef cattle. Food Control. 2001;12:13–25. DOIGoogle Scholar
- Food and Drug Administration Center for Veterinary Medicine. The human health impact of fluoroquinolone resistant Campylobacter attributed to the consumption of chicken [cited 2018 Oct 16]. https://www.fda.gov/downloads/animalveterinary/safetyhealth/recallswithdrawals/ucm152308.pdf
- European Centre for Disease Prevention and Control (ECDC); European Food Safety Authority (EFSA); European Medicines Agency (EMA). ECDC/EFSA/EMA second joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals: Joint Interagency Antimicrobial Consumption and Resistance Analysis (JIACRA) Report. EFSA J. 2017;15:
e04872 .PubMedGoogle Scholar - Carmo LP, Nielsen LR, da Costa PM, Alban L. Exposure assessment of extended-spectrum beta-lactamases/AmpC beta-lactamases-producing Escherichia coli in meat in Denmark. Infect Ecol Epidemiol. 2014;4:1. DOIPubMedGoogle Scholar
- Collineau L, Backhans A, Dewulf J, Emanuelson U, Grosse Beilage E, Lehébel A, et al. Profile of pig farms combining high performance and low antimicrobial usage within four European countries. Vet Rec. 2017;181:657–657. DOIPubMedGoogle Scholar
- Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. DOIPubMedGoogle Scholar
- Hald T, Lo Fo Wong DM, Aarestrup FM. The attribution of human infections with antimicrobial resistant Salmonella bacteria in Denmark to sources of animal origin. Foodborne Pathog Dis. 2007;4:313–26. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. National Antimicrobial Resistance Monitoring System (NARMS): human data [cited 2018 Oct 18]. https://wwwn.cdc.gov/narmsnow
- US Department of Agriculture. Livestock & meat domestic data. Annual historical red meat supply and disappearance and per capita disappearance data [cited 2018 Oct 18]. https://www.ers.usda.gov/data-products/livestock-meat-domestic-data/livestock-meat-domestic-data/#Beef
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey data [cited 2017 Feb 4]. http://wwwn.cdc.gov/nchs/nhanes/search/nhanes03_04.aspx
- Yue S, Pilon P. A comparison of the power of the t test, Mann-Kendall and bootstrap tests for trend detection / Une comparaison de la puissance des tests t de Student, de Mann-Kendall et du bootstrap pour la détection de tendance. Hydrol Sci J. 2004;49:21–37. DOIGoogle Scholar
- Gelman A, Carlin J, Stern H, Dunson D, Vehtari A, Rubin D. Bayesian data analysis, 3rd ed. [cited 2017 Mar 7]. https://www.crcpress.com/Bayesian-Data-Analysis-Third-Edition/Gelman-Carlin-Stern-Dunson-Vehtari-Rubin/p/book/9781439840955
- Dargatz DA, Kopral CA, Erdman MM, Fedorka-Cray PJ. Prevalence and antimicrobial resistance of Salmonella isolated from cattle feces in United States feedlots in 2011. Foodborne Pathog Dis. 2016;13:483–9. DOIPubMedGoogle Scholar
- Williams MS, Ebel ED, Vose D. Methodology for determining the appropriateness of a linear dose-response function. Risk Anal. 2011;31:345–50. DOIPubMedGoogle Scholar
- Williams MS, Ebel ED. Estimating changes in public health following implementation of hazard analysis and critical control point in the United States broiler slaughter industry. Foodborne Pathog Dis. 2012;9:59–67. DOIPubMedGoogle Scholar
- Guillard T, Pons S, Roux D, Pier GB, Skurnik D. Antibiotic resistance and virulence: Understanding the link and its consequences for prophylaxis and therapy. BioEssays. 2016;38:682–93. DOIPubMedGoogle Scholar
- Laufer AS, Grass J, Holt K, Whichard JM, Griffin PM, Gould LH. Outbreaks of Salmonella infections attributed to beef —United States, 1973-2011. Epidemiol Infect. 2015;143:2003–13. DOIPubMedGoogle Scholar
- US Department of Agriculture Food Safety Inspection Service. Risk assessment of lethality standards for RTE meat and poultry [cited 2020 Feb 18]. https://www.fsis.usda.gov/wps/wcm/connect/ace90cc5-2be2-4fa3-9ed5-2b186cae976c/Salm_RTE_Risk_Assess_ExecSumm_Sep2005.pdf?MOD=AJPERES
- Reicks AL, Brooks JC, Garmyn AJ, Thompson LD, Lyford CL, Miller MF. Demographics and beef preferences affect consumer motivation for purchasing fresh beef steaks and roasts. Meat Sci. 2011;87:403–11. DOIPubMedGoogle Scholar
- Bogard AK, Fuller CC, Radke V, Selman CA, Smith KE. Ground beef handling and cooking practices in restaurants in eight States. J Food Prot. 2013;76:2132–40. DOIPubMedGoogle Scholar
- US Department of Agriculture. Feedlot 2011. Part III: Trends in health and management practices on U.S. feedlots, 1994–2011 [cited 2016 Oct 31]. https://www.aphis.usda.gov/animal_health/nahms/feedlot/downloads/feedlot2011/Feed11_dr_Part%20III.pdf
- US Department of Agriculture. Feedlot 2011. Part IV: Health and health management on U.S. feedlots with a capacity of 1,000 or more head [cited 2016 Oct 31]. https://www.aphis.usda.gov/animal_health/nahms/feedlot/downloads/feedlot2011/Feed11_dr_PartIV.pdf
- Brault SA, Hannon SJ, Gow SP, Warr BN, Withell J, Song J, et al. Antimicrobial use on 36 beef feedlots in western Canada: 2008–2012. Front Vet Sci. 2019;6:329. DOIPubMedGoogle Scholar
- Benedict KM, Gow SP, McAllister TA, Booker CW, Hannon SJ, Checkley SL, et al. Antimicrobial resistance in Escherichia coli recovered from feedlot cattle and associations with antimicrobial use. PLoS One. 2015;10:
e0143995 . DOIPubMedGoogle Scholar - Vikram A, Miller E, Arthur TM, Bosilevac JM, Wheeler TL, Schmidt JW. Similar levels of antimicrobial resistance in U.S. food service ground beef products with and without a “raised without antibiotics” claim. J Food Prot. 2018;81:2007–18. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: July 27, 2020
1These authors contributed equally to this article.
Table of Contents – Volume 26, Number 9—September 2020
| EID Search Options |
|---|
|
|
|
|
|
|



Please use the form below to submit correspondence to the authors or contact them at the following address:
Francisco Zagmutt, EpiX Analytics, LLC, 375 E Horsetooth Ave, #2-100, Fort Collins, CO 80525, USA
Top